Current Research in Vision Rehabilitation
Our research faculty are committed to discovering new and innovative ways to improving the lives of patients with low vision and to improving their vision rehabilitation outcomes.
For more information, visit the ultra-low vision lab.
Low vision rehabilitation outcomes and measurement
Dr. Judith Goldstein has spent much of her research career improving the accuracy and precision in measuring visual ability function in patients with low vision. Visual ability is a latent variable and thus, difficult to measure, making comparative clinical research of various interventions problematic. Her research has involved developing a network of physicians to build consensus around a measure and leading the network in a study of changes in visual ability in a large sample of patients across the U.S. Subsequently, Dr. Goldstein collaborated with scientists and mathematicians to calibrate visual function questionnaires to minimize the error observed in measuring patient reported outcomes (PRO’s) in retina diseases and low vision. Currently Dr. Goldstein is collaborating with NEI to examine PRO’s in the Age-Related Eye Disease Study.
Dr. Dominic Brown, Dr. Belinda Weinberg, Dr. Judith Goldstein, and Dr. Chris Bradley are researching the feasibility of developing a methodology to extract, interpret, and analyze a patient's functional history data, as well as offer suggestions for standardizing data recording.
Kristen Shifflett, OTR/L, CLVT is studying ways to improve the rehabilitation process for people with vision impairment using a multi-disciplinary team approach.
Healthcare delivery
More recently, Dr. Goldstein’s work has focused on health care delivery and implementation science — how do we improve connecting patients to low vision care. As few are aware of the availability of services to improve function in the setting of chronic vision loss, it is often the recommendation by the managing ophthalmologist to refer for care; given the high patient volume in ophthalmology care and focus on disease management, referral for rehabilitation is unfortunately often overlooked. Dr. Goldstein and her team developed and piloted the first clinical decision support system in ophthalmology relying on user-centered design and an alert in the health record. This quality improvement work identified several factors predict utilization and connection to low vision services, including an active alert in the electronic health record, endorsement by the referring ophthalmologist to seek care and rehabilitation service provision at the same location where the patient receives their medical eyecare. Next steps of this work are to expand and study the effects of clinical decision support nationally.
Scotomas and visual field loss
Presently Dr. Goldstein is collaborating with other researchers at the Lions Vision Center to build a 3-D system and examine scan paths in patients with central and peripheral vision loss. The aim is to better understand whether training eye movements can enhance visual function, including reading and overall viewing.
Dr. Chris Bradley is developing improved methods for detecting visual field loss and measuring disease severity by testing different statistical approaches on over half a million visual fields stored in the Wilmer Eye Institute database.

"Odd-one-out" task used to collect scan patterns in patients with visual field loss due to stroke while they look for the mismatched object between the left and right sets.
RPB-LCIF hemianopia study: Patients suffering a stroke of the posterior cerebral artery, or similar loss of the blood supply to the visual cortex on one side of the brain, may experience a condition called hemianopia, in which either the left or the right half of the visual field suddenly becomes blind. While their vision in the other half of the field, and so their central detail vision, may be perfectly fine, they will experience great difficulty finding objects and avoiding obstacles or approaching persons or vehicles in the blind hemifield. Some patients overcome this impairment by effective scanning with the head and eyes, learning to be vigilant without major effort. Others, however, remain impaired and seem unable to regain normal function, even with the help of low vision rehabilitation. Our hypothesis is that the latter group fails to acquire effective scan patterns. Sponsored by an award from Research to Prevent Blindness and the Lions Clubs International Foundation, and with the help of Hopkins physicians referring patients and the Low Vision Clinic team providing clinical assessment and rehabilitation, Dr. Gislin Dagnelie and his team are studying scanning patterns in patients with hemianopia, soon after their stroke and as they progress through recovery. Study participants’ eye and head movements are recorded while they perform a series of tests in virtual reality, using a specialized head-mounted display with built-in tracking.
Ultra-Low Vision Lab

Sample image with three different camera modes for the Argus II system - normal Argus II camera (left),stereo camera (center), and a thermal camera (right).
Argus II retinal prosthesis: Argus II is the only FDA approved retinal implant in the United States. It has been implanted in over 300 individuals with retinitis pigmentosa worldwide. Even though Argus II is not commercially manufactured anymore, we continue to collaborate with industry (MinnHealth and Advanced Medical Electronics, Minnesota) and academic partners (Johns Hopkins Applied Physics Laboratory, Columbia, MD) to develop cutting-edge technology and research such as evaluating the efficacy of an AI-based object finder device, image enhancement using stereo and thermal filters and development of a Spatial Localization and Mapping (SLAM) device that can enhance performance for Argus II users.

Normally sighted subject performing a phosphene mapping test under simulated conditions presented in an HTC VIVE Headset.
Intracortical visual prosthesis (ICVP): Dr. Gislin Dagnelie is a co-investigator in the ongoing Intracortical Visual Prosthesis study that is funded by the NIH BRAIN Initiative. The study is based in Chicago with multiple centers – Illinois Institute of Technology, Rush University Medical Center and the Chicago Lighthouse. The first patient was implanted with the cortical prosthesis in early 2022 and Dr. Dagnelie’s team is developing software for psychophysical testing with the ICVP system. This involves direct stimulation and threshold testing of individual electrodes, phosphene mapping and activation of camera mode for real-world use of the device.

Crude phosphene map from the first ICVP subject.
Ultra-low vision toolkit: Apart from the vision restoration therapies mentioned above, there are many other therapies that are under development or in various stages of clinical trials such as stem cell, optogenetic, and gene therapy. These studies recruit people in advanced stages of an eye disease who are blind or have limited vision (ultra-low vision or ULV; seeing light, movement and/or crude shapes, but no details), and even the restored vision may be limited to ULV. Our research aims to understand performance of daily activities with ULV and whether there are ways to improve performance of visually-guided activities. Dr. Dagnelie in collaboration with BaltiVirtual Inc., with funding from the NEI, has designed and developed a toolkit that can be used for assessing visual performance in people with ULV. Dr. Arathy Kartha, a postdoc fellow in the lab, is incorporating these tests in the development of a multisensory training program for people with ULV, funded by an NEI pathway to independence award.
Sample images from the ULV toolkit to assess visual information gathering (WILMER VRI)

1.View of an empty room presented at three different light levels.
2. View of a lit candle on the table under three different levels of background lighting.
3. Place settings with one plate missing, presented on a tabletop at three contrast levels.
Hand-eye Coordination Test in the Ultra-Low Vision Toolkit
Video of a participant performing a hand-eye coordination task, wearing an HTC VIVE Headset and a LeapMotion sensor to track his hand in space.
Ultra-Low Vision Toolkit - Wayfinder Subway Simulation
Data Visualization of a wayfinding task, where participants' movements and gaze are visualized as they navigate a metro station to board a train.
Multisensory Research and Rehabilitation
The XYZ Sensory Lab is conducting research to provide innovative solutions for the real-life functioning of individuals with multiple sensory impairments.
Spatial Localization with Dual Sensory Impairment
Dual sensory impairment (DSI) refers to the co-occurrence of vision and hearing impairment. DSI can be a result of genetic disorders such as Usher Syndrome, or due to age-related sensory decline. Numerous epidemiology research has demonstrated the increased challenges individuals with DSI face in independent living and social life, but there is a lack of system to address the unique rehabilitation needs required by this population. In this research, we translate sensory sciences into clinically feasible survey and performance-based assessment tools to increase the outcomes of vision and hearing rehabilitation services and improve the real-life functioning of individuals with DSI.
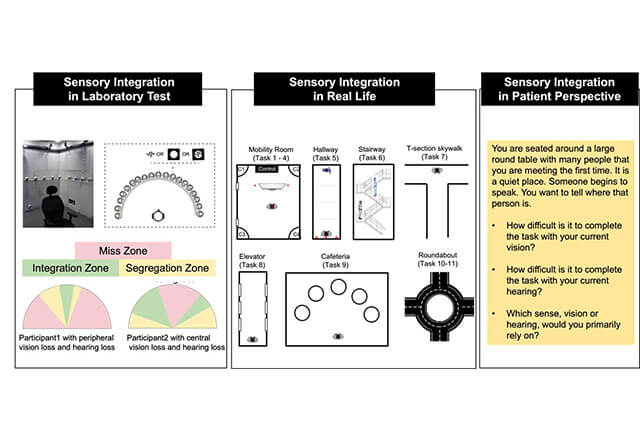
Sensory integration: from laboratory to real-life, and from theory to clinical applications.
Enhancing Visual Accessibility of Indoor Spaces
The visual accessibility of a space refers to the effectiveness with which vision can be used to travel safely and pursue intended activities in the space. Visual accessibility of a space is lower for impaired vision, leading to higher risks of encountering hazardous situations, falling, and being disoriented in navigation. However, it is difficult for people with normal vision, even those with rehab expertise, to judge whether specific objects or features would be visible for individuals with different levels of vision impairment, or to judge the efficacy of modifications. Our research aims to develop an objective tool for Evaluating the Visual Accessibility (EVA) of indoor spaces. Supported by advanced camera and depth sensing technologies and modern computer vision algorithms, EVA will be implemented as a smartphone app for easy use by rehab specialists and the general public.
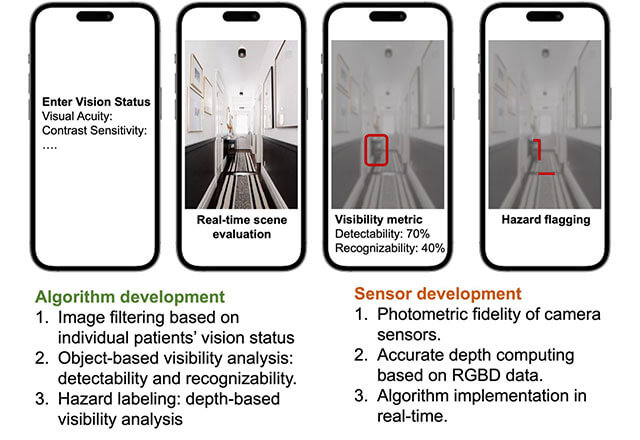
A conceptual demonstration of EVA: real-time visibility evaluation for environmental features based on any specified level of vision impairment.


