US Family Health Plan and Medicare
For Providers at a glance
Providers are required to check US Family Health Plan beneficiaries’ identification cards in order to verify their eligibility.
The information on the back of the membership card can assist a member in case of emergency. It also gives the health care provider valuable claims processing information.
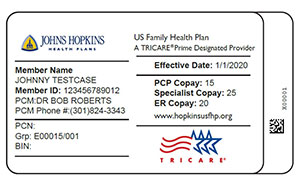
View enlarged image.
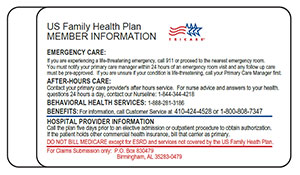
View enlarged image.
MEMBERS NEED TO CARRY THIS CARD AT ALL TIMES.
For beneficiaries who have coverage under both the US Family Health Plan and Medicare:
- Medicare cannot be billed for services which are covered by the US Family Health Plan.
- Beneficiaries filing Medicare claims, or who have claims filed on their behalf, are in violation of the conditions of participation for the US Family Health Plan and are subject to disenrollment.
- Beneficiaries who have coverage under both the US Family Health Plan and Medicare may only use Medicare benefits for non-covered US Family Health Plan services, such as chiropractic care.
- Beneficiaries utilizing Medicare for benefits covered under TRICARE Prime are subject to disenrollment.
