Stem Cell Research at Johns Hopkins Institute of Basic Biomedical Sciences
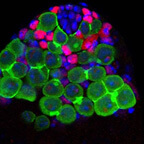
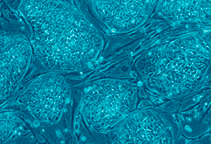 Image by Nissim Benvenisty
Image by Nissim BenvenistyResearchers at the IBBS are studying stem cells to figure out how they can give rise to a complex body, how cells of the body can revert back to stem cells and how this knowledge can be used to develop therapies for diseases and injuries.
Stem cells are cells that don’t have an identity but have the potential to develop into many types of cells for many purposes, liking building a complete organism, healing a wound or replacing old, worn-out cells in a tissue.
Embryonic stem cells can become any of the cells in the body and can form entire animals.
Not all stem cells come from embryos, adult stem cells are found throughout the body too. These cells don’t have the ability to become any cell in the body, but can transform into many different cell types. For instance, there are stem cells in our bone marrow that can become fat cells, cartilage cells or bone cells, but they can’t become eye cells or skin cells. Researchers have also figured out how to make adult cells, like a skin cell, turn back into cells with the properties of embryonic stem cells, called induced pluripotent stem cells or iPS cells for short.
Erika Matunis, in the Department of Cell Biology, studies in fruit flies how testis stem cells decide to stay stem cells and not become other cell types, like sperm. She has also discovered how cells that are turning into other cell types can revert back to stem cells if the permanent reservoir of stem cells is depleted and she is exploring the mechanism of how this happens. Her research, learning more about the most fundamental aspects of stem cell biology, helps all stem cell researchers better understand the cells they work with.
Jennifer Elisseeff, of the Department of Biomedical Engineering, studies the differences between embryonic stem cells and adult stem cells. She has found that embryonic stem cells are better at forming new tissues, whereas adult stem cells are better at secreting therapeutic molecules that promote healing of damaged tissue. Elisseeff is particularly interested in the factors released by stem cells that can help a tissue heal. She uses this information in the development of biosynthetic (part-natural and part-man-made) materials used for therapies. One of the materials her lab has developed is a bio-adhesive—essentially a glue that can be used in the body that is made of part synthetic and part natural components. The glue is used in conjunction with stitches to help prevent leakage of blood or fluids, but it’s flexible enough to allow cells to move in and heal the incision. Also, Elisseeff is collaborating with the military to develop a treatment for soft tissue facial reconstruction for people who have suffered severe trauma. They are developing tissue blueprints that can be transplanted in the face—or any other place in the body for that matter— that would allow a person’s own cells to move into a region to heal and restructure the tissue.
Warren Grayson, of the Department of Biomedical Engineering, takes stem cells from fat and bone marrow as well as stem cells that have the potential to become many different cell types, known as pluripotent stem cells, and coaxes them to regenerate bone or skeletal muscle in the lab. He does this by incubating stem cells in biosynthetic structures to give the cells a structured three-dimensional volume to grow in, and then places these either in bioreactors that provide heat, nutrients, movement, mechanical stress or control of any other condition like oxygen concentration to guide the stem cell to become a specific cell type or within a defect in animals to study the regenerative process. He hopes to one day be able to take a person’s own stem cells and grow tissues, like bone or muscle, to be implanted into their body to replace damaged tissue. Using a person’s own cells and tissues will reduce the likelihood that the transplanted tissue will be rejected by the immune system.
Related Links: Stem Cell Research at Johns Hopkins
