Accomplishments
Advancements in High-Value Health Care
Johns Hopkins is renowned as the home of some of the world’s most talented and innovative minds in medicine and science. Several groups of our doctors and administrators are turning their talents toward refining care delivery to help patients stay healthier. Here is a look at the progress we’ve made over the last decade.
Second Three-Year Grant Awarded
The High Value Practice Academic Alliance wins a second three-year grant from the Agency for Health Care Research and Education to conduct its annual care conference.
Creating a Clinically Integrated Network
Johns Hopkins Medicine creates the Johns Hopkins Clinical Alliance, a physician-led network aimed at supporting value-based care delivery, under the guidance of Sarah Johnson Conway , chief medical officer.
Collaborating with Baltimore Medical System to Become an FQHC
East Baltimore Medical Center is transitioned to a Federally Qualified Health Center (FQHC) under Baltimore Medical System. The transition represents a unique collaboration bringing together an academic medical center and FQHC in the care of the local community, combining unique resources afforded by BMS with the clinical and academic acumen of Johns Hopkins Medicine.

Developing Appropriate Use Criteria for Diagnostic Imaging
Johns Hopkins Medicine receives approval to set our own standard of care for imaging and other diagnostic decision-making, tailored to the various practice settings and in line with government regulations. This approval from the Centers for Medicare & Medicaid Services (CMS) means Johns Hopkins is a CMS-qualified provider-led entity, with delegated authority to write appropriate use criteria for imaging. Our criteria and guidelines are derived from the strongest evidence in medical literature, under the direction of teams of clinical experts from each entity in the health system.
Funding for Evidence-Based Care Initiative
The Strategic Priority Executive Council funds a three-year project to integrate diagnostic and management decision-making evidence-based guidelines into the electronic medical record across the health system. This project is designed to increase quality, safety, efficiency and affordability of care and improve outcomes.
Building Value Through Patient-Centered Care
Johns Hopkins Medicine Alliance for Patients (JMAP) joins the Centers for Medicare & Medicaid Services to become a care transformation organization . The agreement brings patient-centered care to Maryland’s Medicare fee-for-service patients. JMAP transforms care through customizable care delivery, information technology and quality improvement that adds value.
Center for Innovative Medicine
Johns Hopkins Center for Innovative Medicine awards Pamela Johnson five years of support as the Stanley Levenson Scholar to advance high-value performance improvement across the health system and the country.
Using "Virtual Patients" to Train Doctors
A new, online, case-based education module from the Johns Hopkins University School of Medicine basic medicine clerkship teaches third-year medical students how to order medical tests appropriately.
Created by hospitalists Amit Pahwa and Leonard Feldman , the Hopkins Virtual Patient lets students evaluate three hypothetical patients and select tests. The test choices include Medicare fees or average wholesale prices. Users get insights on Maryland’s Global Budget Revenue, including its fee and reimbursement policies.
Teaching Value Innovation Awards
Johns Hopkins-directed High Value Practice Academic Alliance wins Teaching Value Innovation Awards from Costs of Care/ABIM Foundation for graduate medical and CME educational programs.
Three-Year Grant Awarded
The High Value Practice Academic Alliance wins a three-year grant from the Agency for Health Care Research and Education to conduct its annual care conference.
High Value Practice Academic Alliance Approved
The High Value Practice Academic Alliance is approved by the Centers for Medicare & Medicaid Services as a qualified provider-led entity to develop advanced imaging appropriate use criteria and for sharing the criteria with others.
2018 Teamwork Award in Quality Improvement
The Johns Hopkins Health System’s High Value Care Committee receives the 2018 Teamwork Award in Quality Improvement from the Society of Hospital Medicine.

Speeding Best Practice Evidence to Patients and Doctors
When a patient comes to The Johns Hopkins Hospital’s emergency department, time is everything. Now our doctors can easily access the latest treatment regimen and tailored patient instructions, right through the electronic medical record system. Doctors can now see the latest best practice from >100 common conditions, such as chest pain, abdominal pain and dizziness. Calculators and flow charts help physicians pinpoint the best course of action and tailor that care to the particular patient.
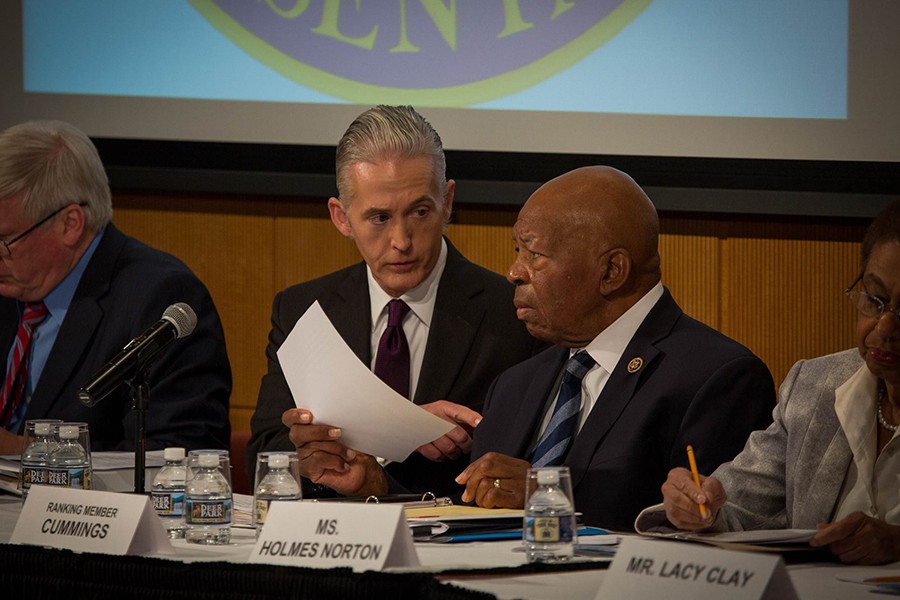
Fighting the Opioid Epidemic
Johns Hopkins experts across the health system work to avoid opioid over-prescription while addressing effective pain management. Tasks focus on pain management before, during and after surgery; educating medical and nursing students on pain; establishing guidelines and creating an inpatient pain treatment program. At a congressional hearing held at The Johns Hopkins Hospital on Nov. 28, 2017, Rep. Elijah Cummings, ranking member of the U.S. House Committee on Oversight and Government Reform, notes Johns Hopkins’ leadership in combatting the problem.
2017 Innovations in Clinical Care Award
Pamela Johnson, Lenny Feldman, Amit Pahwa and the High Value Care Committee receive the 2017 Innovations in Clinical Care Award from Johns Hopkins Medicine for successfully improving appropriateness of tests across the health system and launching a national high-value academic collaborative to improve care broadly.

Forming a National Consortium of High-Value Care Leadership
The Johns Hopkins University School of Medicine forms a consortium of academic medical centers across the country to advance high-value medical practice through research, innovation, collaboration and education. The High Value Practice Academic Alliance is established by Roy Ziegelstein , vice dean for education, and Lenny Feldman and Amit Pahwa , co-directors of the Department of Medicine High Value Care Committee.
Creating a Center to Reduce Diagnostic Errors
Johns Hopkins Medicine opens the Armstrong Institute Center for Diagnostic Excellence to enhance diagnostic accuracy, cut waste on unnecessary diagnostic testing, and move the needle on eliminating preventable harms from diagnostic errors worldwide. The center, led by David Newman-Toker , professor of neurology and otolaryngology and an internationally-recognized leader in diagnostic research and diagnostic safety, is part of the Johns Hopkins Armstrong Institute for Patient Safety and Quality .
Cutting Costs, Improving Care Across the Health System
The Johns Hopkins Health System High Value Care Committee forms to improve patient care quality and cut wasteful practices. Representatives from all five regional hospitals and Johns Hopkins Community Physicians practices come together to refine diagnostic testing. It is an outlet through which professionals share successes and discuss opportunities to optimize resource use.
Involving Graduate Medical Trainees and Medical Students in Reducing Unnecessary Treatments
The High Value Practice Alliance, a committee of faculty educators and quality leads from multiple departments, engages residents and fellows in reducing unnecessary tests and treatments. Faculty members in radiology, emergency medicine, internal medicine, neurology and other specialties identify improvement projects for student involvement.
In one project, emergency medicine residents determine that coagulation studies are not helpful in caring for patients with chest pain. They add a pop-up message advising on best practices in the electronic health record, reducing orders for the test and saving about $50,000 for the health system.

Connecting Patients and Reducing Readmissions
The After-Care Clinic , located at the Johns Hopkins Outpatient Center on the East Baltimore campus, offers multidisciplinary post-discharge care to adult patients identified as high risk for readmission or emergency department use. In 2016, the After-Care Clinic saved the health system about $1.4 million.

Calling Patients and Families to Clarify Care Orders
The Johns Hopkins Hospital Patient Access Line (PAL) connects with patients after discharge to reinforce key aspects of self-care. Each patient gets a timely follow-up phone call from a Johns Hopkins nurse. Using information from Epic electronic medical records and several other databases and systems, the nurse answers any questions and makes sure that each patient understands the care directions. Over a three-year study period, patients who did not connect with PAL experienced a 45% greater chance of readmission than patients who used PAL.

Identifying Low-Yield, gh-Cost Tests
The Department of Medicine esta ishes the High Value Care Committee to reduce unnecessary tests a treatments that add costs without helping doctors make cisions. Doctors, nurses, administrative staff members d medical students look at areas where the department ca reduce tests for folate, telemetry use, asymptomatic b teriuria and other screenings.

Diagnosing Stroke for Less
The emergency department at The Johns Hopkins Hospital uses a special pair of goggles to assess patients for stroke and rule out other causes for symptoms. The goggles, which are found to decrease ER wait times, diagnose stroke with 100% accuracy. Using the goggles eliminates a large portion of the roughly $9 billion spent on evaluating and diagnosing patients with stroke in the emergency room. And, fewer people suspected of having a stroke are unnecessarily admitted to the hospital.
Creating an Accountable Care Organization
Johns Hopkins Medicine creates the Johns Hopkins Medicine Alliance for Patients, a Medicare shared savings program accountable care organization, to increase value and access for patients across Maryland.
Led by cardiologist Scott Berkowitz , the alliance seeks to provide the right care for the right patient at the right place and at the right cost by focusing efforts in the key areas proven to be essential for successful population health management. The group has received a high quality rating from the Centers for Medicare & Medicaid Services, reducing readmissions and decreasing emergency department visits for its more than 39,000 beneficiaries.

Helping Doctors Choose Wisely
Roy Ziegelstein , the Johns Hopkins University School of Medicine’s vice dean for education, initiates a campaign to identify commonly used tests and procedures no longer considered the gold standard for care. The Choosing Wisely initiative asks program directors across the school of medicine to work in their specialty area along with residents and fellows to reduce or eliminate unnecessary or wasteful procedures. The campaign targets 40 specialty-based tests and procedures .

Less Blood = Shorter Hospital Stays, Fewer Readmissions
Based on 10 scientific studies and AABB clinical practice guidelines, Johns Hopkins launches a program to reduce the amount of blood used in transfusions. Within six years, The Johns Hopkins Hospital reduces hospital stays after blood transfusion from three days to just two. At the same time, the campaign lowers the risk for readmission within 30 days of discharge from 9% to 5.8%.

Creating a Bridge to Health After Heart Failure
The Heart Failure Bridge Clinic opens to address the care needs of patients with heart failure. In 2019, the clinic handles about 2,500 outpatient visits a year, and has reduced the hospital readmission rate for patients to 8.6% (the national readmission rate is about 25%).

Creating Medical Communities to Redefine Standard Care
The first Clinical Communities comprise physicians from across the five Johns Hopkins Baltimore- and Washington-area hospitals. Their goal is to deliver superior care efficiently in each of their respective specialty areas, and bring best practices to their hospitals.
Together, these groups standardize care and reassess all costs associated with care delivery. As of 2019, more than 20 communities have explored issues such as blood management, care in the neonatal intensive care unit and maternity services.
Empowering Patients After Discharge
The Transition Guide Nurses Program at Suburban Hospital is initiated to help patients better understand their wound care, medication schedules and follow-up appointments after discharge. Nurses call patients to reinforce key aspects of self-care and to explain signs and symptoms that may require a visit to the patient’s primary care physician.

Keeping Elderly Patients Safe After Discharge
Physicians at Johns Hopkins Bayview Medical Center establish Safe and Successful Transition of Elderly Patients ( Safe STEP ). The pilot, led by internist Eric Howell and Steven Kravet , president of Johns Hopkins Community Physicians, reduces readmission rates at 30 days after discharge from 22% to 14%, and cuts emergency room visits three days after discharge from 10% to 3%.
Reducing Tests Saves Money, Time and Needles
A group of concerned internal medicine residents and faculty members at Johns Hopkins Bayview Medical Center founds Providers for Responsible Ordering to educate doctors about appropriate lab ordering and blood draws. Within two years, the team shares results showing a 66% reduction in cardiac-enzyme tests, saving $1.3 million. In 2011, the group is one of only five medical organizations to receive an ABIM Foundation Putting the Charter Into Practice grant, in recognition of its efforts to “provide health care that is based on the wise and cost-effective management of limited clinical resources.”

