Meniscal Transplant Surgery
What is meniscal transplant surgery?
Meniscal transplant surgery is a type of surgery that replaces your missing or damaged meniscus with a meniscus from a cadaver donor. The surgery usually takes place under general anesthesia.
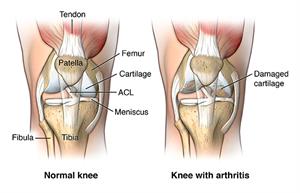
Your knee has 2 wedge-shaped pieces of cartilage, 1 on each side of your knee. Each one of these pieces is called a “meniscus.” These 2 rubbery menisci act as shock absorbers between your thighbone (femur) and your shinbone (tibia). A different type of cartilage capping the tibia and femur also helps your bones move smoothly. These 2 menisci help protect the ends of your femur and tibia as they move together.
Sometimes, a twisting injury may severely damage your meniscus. If the damage is severe enough, your surgeon may need to remove your meniscus. Without this meniscus cushion, the ends of your tibia and femur may start to rub together abnormally. Over time, this can cause persistent knee pain. Eventually, it may cause arthritis. Your cartilage “cap” degrades and the bones beneath start to scrape together.
Meniscal transplant surgery provides another choice for you. Your surgeon makes a very small incision in your knee. He or she uses special instruments and cameras to access the joint space between your femur and tibia. Next, your surgeon surgically sews the donated meniscus into your joint space.
Meniscus Tear| Grace's Story
Why might I need meniscal transplant surgery?
Meniscal transplant surgery might make sense for you if your meniscus was removed in a previous surgery. (This probably happened if the damage to your meniscus was so bad that surgeons couldn’t repair it in that previous surgery.) Without a meniscus, you might gradually develop knee pain and arthritis of your joint. Replacing your meniscus may provide significant pain relief. It may also help prevent arthritis in your joint. This can develop when your cartilage becomes frayed and rough. This surgery is less invasive than knee replacement surgery.
Meniscal transplant surgery might not make sense for you, even if you’ve had your meniscus removed. If you already have arthritis of your knee, the procedure might not help because you may already have too much damage to your cartilage and bone. Another procedure, like knee replacement, might be more effective.
You might be a good candidate for meniscal transplant surgery if the following apply to you:
-
You’re younger than age 55.
-
You’re missing more than half your meniscus, or you have a large meniscus tear that is irreparable.
-
You have significant or persistent pain with activity, or you have an unstable knee.
-
You have only minimal arthritis, or none at all.
-
You have a knee with normal alignment and stable ligaments.
-
You are not obese.
What are the risks of meniscal transplant surgery?
Most people have meniscal transplant surgery without any problems. Rarely, complications happen, like:
-
Stiffness of the joint after surgery (more common)
-
Incomplete healing. This might need another surgery.
-
Excess bleeding
-
Infection
-
Damage to nearby nerves
-
Complications from anesthesia
-
Getting an infection from the donated tissue (extremely rare)
Your own risks may vary according to your age, your other medical conditions, and the specific anatomy of your knee. Talk with your surgeon about your concerns. Make sure you include the risks that most apply to you.
How do I get ready for a meniscal transplant surgery?
Talk with your healthcare provider about how to prepare for your meniscal transplant surgery. Ask whether you should stop taking any medicines ahead of time, like blood thinners. Tell your healthcare provider about all the medicines you take, including over-the-counter medicines like aspirin. You’ll need to avoid food and drink after the midnight before your procedure.
Before your procedure, you may need additional imaging tests, like X-rays and magnetic resonance imaging (MRI).
You may need to rearrange your living arrangements as you recover because you’ll need to use crutches for several weeks.
You may be able to go home on the day of your surgery. It’s also possible you’ll need to stay in the hospital for a day or two. Talk with your healthcare provider ahead of time so that you can make the necessary arrangements for your recovery period.
Before your surgery, a healthcare provider will carefully screen the donated meniscus for any signs of infection.
What happens during meniscal transplant surgery?
Your healthcare provider can help explain the details of your particular surgery. An orthopedic surgeon will perform the surgery. The whole operation may take a couple of hours. In general, you can expect the following:
-
A healthcare provider (anesthesiologist) will give you medicine so that you’ll sleep through the operation and won’t feel any pain or discomfort during the surgery. (You may receive spinal anesthesia and a medicine to help you relax.)
-
Your vital signs, like your heart rate and blood pressure, will be monitored during the operation. You may have a breathing tube inserted down your throat during the operation to help you breathe.
-
After cleaning the affected area, your surgeon will make a small incision through the skin and muscle of your knee.
-
Your healthcare provider will insert a very small camera through this incision, using this camera to guide the surgery.
-
Using very small instruments inserted through the incision, your surgeon will remove any remaining meniscus.
-
Next, he or she will surgically sew the donated meniscus into the joint space. The healthcare provider might use screws or other devices to hold the meniscus in place.
-
Your surgeon will make other repairs, if necessary.
-
The surgeon will close the layers of skin and muscle around your knee.
What happens after meniscal transplant surgery?
Talk with your healthcare provider about what you can expect after your surgery. In some cases, you may be able to go home a few hours after your surgery. (If so, make sure you have someone who can drive you home.) In other cases, you may need to stay overnight at the hospital for monitoring.
You may have some pain right after your surgery, but pain medicines may help to ease the pain. The pain should quickly begin to diminish, and you should have less pain than before your surgery.
After your surgery, you will probably need to wear a knee brace for a few weeks. You might also need to use crutches during this time. Your healthcare provider will give you instructions about how you can move your knee while you recover. You might need physical therapy for a few months to help you maintain your strength and range of motion. It may be several months before you can return to all your previous activities.
You may have some fluid draining from your incision, which is normal. Let your healthcare provider know right away if you see an increase in redness, swelling, or draining from your incision, or if you have a high fever, chills, or severe pain.
Make sure to keep all your follow-up appointments, so your healthcare provider can monitor your progress. Following all of your healthcare provider’s instructions may increase your chances for a positive outcome.
Next steps
Before you agree to the test or the procedure make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how will you get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much will you have to pay for the test or procedure