Minimally Invasive Total Knee Replacement
What is a total knee replacement?
Total knee replacement is a type of surgery to replace a damaged knee joint. A minimally invasive surgery uses a smaller cut (incision) than a traditional total knee replacement. This type of surgery typically requires special tools so that the surgery team can see and do the procedure through the smaller incision.
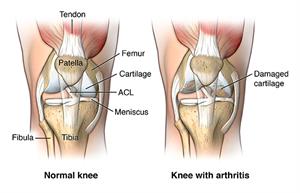
The knee has several parts: the lower end of the thigh bone (femur), the upper end of the shin bone (tibia), and the kneecap (patella). A smooth substance called cartilage caps the ends of these bones and keeps the bones from grinding together. When there is damage to the knee joint, these bones may scrape together abnormally and cause pain.
During minimally invasive total knee replacement, your surgeon makes an incision to access your shinbone and thigh bone. Next, he or she removes a portion of the bones that make up the knee joint. Your surgeon replaces these bone parts with metal components that recreate the joint surface. A layer of plastic is placed between the metal components for smooth gliding.
Minimally invasive total knee replacement often takes place under general or spinal anesthesia.
Knee Replacement Surgery | Q&A with Savya Thakkar, M.D.
An expert in hip and knee replacement surgery, Savya Thakkar discusses common reasons for knee replacement, the procedure, the types of implants and recovery.
Why might I need a total knee replacement?
You might need a total knee replacement if you have significant damage to your knee joint. Different types of medical conditions can damage this joint, such as:
-
Osteoarthritis (most common)
-
Rheumatoid arthritis
-
Osteonecrosis
-
Injury or fracture of the knee joint
-
Bone tumor in the knee joint
This damage might be very painful and limit your normal activities. The procedure may help decrease your pain, improve your joint mobility, and quality of life. Usually, healthcare providers only recommend total knee replacement when you still have significant problems after trying more conservative treatments, like pain medicines and corticosteroid shots (injections).
Talk with your doctor about the benefits and risks of having minimally invasive total knee replacement instead of traditional total knee replacement. Minimally invasive total knee replacement uses a smaller incision than a traditional knee replacement, so it may lead to less pain and decreased recovery time. It is not yet clear whether the procedure leads to an increased risk of certain complications, though.
In some cases, you may have other surgical options, like shortening the bone or a partial knee replacement. Talk with your doctor about the risks and benefits of all your options.
What are the risks of total knee replacement?
Most people do very well with their minimally invasive total knee replacement. But as with any surgery, the procedure does carry some fairly rare risks. Possible complications of the surgery include:
-
Infection
-
Excess bleeding
-
Blood clots
-
Injury to nearby nerves
-
Loosening of the components of the knee
-
Limited motion of the knee
There is also a very slight risk that the procedure might not relieve your pain. Your own risk of complications may vary according to your age and your other medical conditions. Ask your provider about the risks that most apply to you.
Pre-Operative Education

How do I get ready for total knee replacement?
Ask your provider how you should plan to get ready for your surgery.
Tell your provider about any medicines you are taking, including:
-
All prescription medicines
-
Over-the-counter medicines such as aspirin or ibuprofen
-
Street drugs
-
Herbs, vitamins, and other supplements
Ask if there are any medicines you should stop taking ahead of time, like blood thinners.
If you smoke, try to quit before your surgery.
If you are overweight, your provider may advise you to try to lose weight before your surgery.
Don’t eat or drink after midnight the night before your procedure.
You may want to make some changes to your house, to make your recovery smoother. This includes things like adding a handrail in your shower.
In some cases, your provider might want additional tests before you have your surgery. These might include:
-
X-rays, to get information about your hip
-
MRI, to get more detailed information about your hip
-
Electrocardiogram (ECG), to make sure your heart rhythm is normal
Follow any other instructions from your healthcare provider.
What happens during total knee replacement?
Your provider can help explain the details of your particular surgery. An orthopedic surgeon will perform the surgery aided by a team of specialized healthcare professionals. The whole procedure may take a couple of hours. In general, you can expect the following:
-
Most likely, you will be given spinal or general anesthesia so that you’ll sleep through the surgery and won’t feel any pain or discomfort during the procedure. Or you may receive local anesthesia and a medicine to keep you relaxed but awake.
-
A healthcare professional will carefully watch your vital signs, like your heart rate and blood pressure, during the surgery.
-
You may receive antibiotics, during and after the procedure, to help prevent infection.
-
Your surgeon will make an incision over the middle of your knee, cutting through your skin and underlying tissue.
-
He or she will remove the damaged portions of your thigh and shin bone, removing a little of the bone beneath as well.
-
Next, metal implants are placed into the joint space, usually cementing them into the remaining bone.
-
In most cases, your surgeon will also remove part of the underside of the kneecap.
-
A plastic spacer is inserted into the space between the metal implants, for ease of movement.
-
The layers of your skin and muscle will be surgically closed.
What happens after total knee replacement?
Talk with your healthcare provider about what you can expect after your surgery. You may have significant pain around your incision after your procedure, but pain medicines may help to relieve your pain. You should be able to get back to a normal diet fairly quickly.
You may get imaging, like an X-ray, to see the results of the surgery. You might be able to go home within a day or two.
Your provider will let you know when you can put weight on your leg. You may have specific instructions about limiting your movements. You might need to use a cane, walker, or crutches for a few days or weeks. A physical therapist can help you maintain your range of motion and strength. You should be able to go back to most light activities within a few weeks. During this time, you may find it helpful to have some extra help at home.
You might have some fluid draining at the incision site. This is normal. Let your provider know right away if you have an increase in redness, swelling, or draining at the incision site. You should also let your provider know if you have a high fever, chills, or severe pain that does not improve.
Make sure to keep all of your follow-up appointments with your surgeon. You may need to have your stitches or staples removed a week or so after your surgery.
Most people note a significant decrease in their pain following a total knee replacement. You may have some remaining stiffness in the joint, as well as more limited range of motion.
The mechanical parts of your knee may wear out or loosen over time. Because of this, you may need revision surgery at some point. But most people will still have functioning knee replacements 15 years after their surgery. You may be able to extend the life of your implant through regular low-impact exercise, while avoiding high-impact exercise (like jogging), and taking precautions to avoid falls.