Knee Arthritis
What You Need to Know
- Knee arthritis occurs when the cushioning cartilage in the joint wears down, making the knee stiff and painful with certain movements.
- Osteoarthritis — gradual, age-related degeneration of cartilage — is the most common form of arthritis in the knee, but trauma and autoimmune conditions can also lead to cartilage damage.
- The cartilage damage associated with arthritis is irreversible, but there are nonsurgical and surgical treatments that can help reduce pain, increase joint flexibility and improve overall quality of life for people with knee arthritis.
What is knee arthritis?
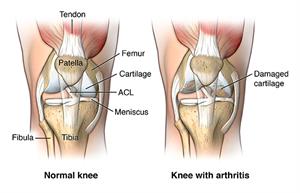
Knee arthritis is inflammation and deterioration of knee joint cartilage. Cartilage is the slippery coating on the ends of bones that serves as a cushion and allows the knee to smoothly bend and straighten. Knee cartilage coats the end of the thighbone (femur), top of the shinbone (tibia) and the backside of the kneecap (patella). When cartilage wears away, the space between the bones narrows. In advanced arthritis, bone rubs on bone and bone spurs (bumps on the bone) may form.
Damage to the joint cartilage over time may result in the development or worsening of deformities of the knee, including knock knees and bowleg.
Where can arthritis occur in the knee?
Cartilage loss can occur between the thighbone and the shinbone in the medial portion (inner side), lateral portion (outer side) and under the kneecap.
- Thinning of the cartilage under the kneecap (patella) is called patellofemoral arthritis (kneecap arthritis).
- Some patients have cartilage loss in one, two or all of these areas. When all three areas are affected, this is called tricompartmental arthritis.
Types of Knee Arthritis
There are many different kinds of arthritis, but the ones most likely to affect the knee are osteoarthritis, rheumatoid arthritis and post-traumatic arthritis.
Osteoarthritis of the Knee
Osteoarthritis is also known as degenerative joint disease. It is the most common form of knee arthritis and can affect other joints as well. It is often associated with wear and tear related to aging, and gradually progresses over time. The breakdown of cartilage leads to pain and inflammation.
Rheumatoid Arthritis of the Knee
Rheumatoid arthritis (RA) is an autoimmune disease in which the immune system attacks healthy tissue in several joints of the body, including the knee. It causes inflammation of the synovial membrane, the capsule surrounding the knee joint. Inflammatory cells release substances that break down knee cartilage over time. Rheumatoid arthritis can affect people of any age.
Post-Traumatic Knee Arthritis
A history of injury or trauma to the knee may lead to development of arthritis. Injuries to the ligaments of the knee make the joint less stable over time, which may lead to cartilage breakdown.
Seminar Management of Knee Arthritis

Knee Arthritis Symptoms
Knee arthritis can make activities of daily living very difficult, including walking and climbing stairs. Signs of arthritis in the knee may include:
- Pain in the knee that can be worsened by certain movements and exercises, including prolonged walking or standing.
- Stiffness of the knee joint, which makes it difficult to bend and straighten the knee.
- Catching and locking of the knee, which occurs when damaged and rough cartilage makes smooth movement difficult.
- Crepitus: the audible cracking, crunching, clicking or snapping sound made when moving a damaged joint.
- Weakness in the knee, which is often a result of reduced activity and resulting atrophy (wasting) of the quadriceps or hamstring muscles. Knee arthritis may reduce how much someone moves, which makes the joint even weaker and worsens symptoms.
Risk Factors for Knee Arthritis
- Age. Osteoarthritis is a degenerative, “wear and tear” condition. The older you are, the more likely you are to have worn-down knee joint cartilage.
- Heredity. Slight joint defects or double-jointedness (laxity) and genetic defects may contribute to osteoarthritis in the knee.
- Excess weight. Being overweight or obese puts additional stress on the knees over time.
- Injury. Severe injury or repeated injury to the knee can lead to osteoarthritis years later.
- Overuse. Jobs and sports that require physically repetitive motions that place stress on the knee can increase risk for developing osteoarthritis.
- Gender. Postmenopausal women are more likely to have osteoarthritis than men.
- Autoimmune triggers. While the cause of rheumatoid arthritis remains unknown, triggers of autoimmune diseases are still an area of active investigation.
- Developmental abnormalities. Deformities such as knock knee and bowleg place higher than normal stress on certain parts of the knee joint and can wear away cartilage in those areas.
- Other health conditions. People with diabetes, high cholesterol, hemochromatosis (high levels of iron in the blood) and vitamin D deficiency are more likely to have osteoarthritis.
How is knee arthritis diagnosed?
Your doctor may use some of the following diagnostic tests and procedures to determine if you have knee arthritis:
- Medical history and physical examination
- Blood tests for genetic markers or RA antibodies
- X-rays to determine cartilage loss in the knee
- Joint aspiration: drawing out and testing the synovial fluid inside the knee joint
Cartilage cannot be seen on X-ray, but narrowing of the joint space between the bones indicates lost cartilage. X-rays show bone spurs and cysts, which can be caused by osteoarthritis. Other tests such as MRI or CT scans are rarely needed for diagnosis.
Knee Arthritis Treatment
Treatment plans vary depending on the type and stage of arthritis, your age, severity of pain and other factors. Cartilage loss cannot be reversed, but there are ways to reduce pain and prevent further damage. Nonsurgical treatments of knee arthritis include:
- Activity modifications that may keep joint pain and inflammation from flaring. This may include avoiding high-impact exercise, such as running and jumping. Engaging in low-impact exercises and remaining physically active is key to managing symptoms.
- Physical therapy to improve strength and range of motion.
- Weight loss (if applicable) to reduce stress placed on the joint.
- Bracing to provide more stability to the joint.
- Medications and injections, such as hyaluronic acid injections, to control pain and inflammation and promote healing.
- Walking aids such as a cane or walker that provide support.
The progression of knee arthritis and effectiveness of nonsurgical treatments varies. Your doctor will work with you to develop a personalized plan that may include a combination of nonsurgical treatments.

Knee Replacement Alternatives to Consider
Before surgery, there are many alternatives to try that could help ease and lessen the pain caused by hip arthritis. Our expert discusses some tips that could reduce the pain and keep you active.
Knee Arthritis Surgery
If nonsurgical treatments don’t provide adequate pain relief and improve mobility, it may be time to discuss surgical options with your doctor, such as:
- Radiofrequency ablation to prevent pain signals from reaching the brain.
- Total knee replacement to resurface the bones in the knee joint with artificial implants to provide more long-term stability and pain reduction.
- Partial knee replacement/resurfacing to address cartilage damage in a small part of the knee.
- Synovectomy to remove the lining of the joint damaged by rheumatoid arthritis.