Heart Failure
What is heart failure?
Heart failure is a condition that occurs when the heart can’t pump as well as it should. This may happen when the heart muscle becomes weak or stiff. As a result, it doesn’t deliver enough blood to the rest of the body. When the body doesn’t get enough blood, it doesn’t get enough oxygen and nutrients.
Heart failure can become life-threatening, so the condition requires medical attention.
What You Need to Know
- Cardiomyopathy, a name for any disease of the heart muscle, is one condition that often leads to heart failure.
- Symptoms of heart failure include shortness of breath, swelling in the legs and feet, and abdominal pain or nausea.
- Diagnosis includes tests for the existence of heart failure, followed by tests to evaluate the cause of the heart failure.
- Treatment for heart failure begins with lifestyle changes and medications. In more advanced cases, surgery may be needed.
- People can and do live with heart failure. Close self-monitoring and sticking to the doctor’s recommended diet, medication and exercise plans are essential to improving quality of life.
What causes heart failure?
Heart failure is usually caused by another health problem. The three most common causes of heart failure are:
- Coronary artery disease: This occurs when the arteries that supply blood to the heart muscle become narrow, causing the heart to work harder to pump blood. Eventually, coronary artery disease can weaken the heart muscle and affect the heart’s pumping ability.
- Heart attack: A heart attack (myocardial infarction) can cause scar tissue that interferes with the heart’s ability to pump. Heart attacks are usually caused by blockages in the heart’s arteries.
- High blood pressure: Also called hypertension, this increased pressure on the artery walls can lead to heart failure.
Other heart failure causes include:
- Arrhythmias: An irregular heartbeat can affect the heart’s ability to pump effectively.
- Cardiomyopathy: This is a disease in the heart muscle that makes the heart less able to pump blood effectively. Several conditions can cause cardiomyopathy, including amyloidosis and sarcoidosis.
- Congenital heart defects: Structural problems in the heart that are present from birth.
- Diabetes: Complications of diabetes can lead to heart failure.
- Infection: A previous infection, such as endocarditis, myocarditis or rheumatic fever, can lead to heart failure.
- Lung disease: Examples include chronic obstructive pulmonary disease (COPD), emphysema or pulmonary embolism (blood clot in the lungs). Lung conditions often cause low oxygen levels. Low oxygen can put extra strain on the heart, weakening it and possibly leading to heart failure.
In addition, some medications can worsen heart failure or interfere with heart medicines, including:
- Certain anti-arrhythmic medications
- Ibuprofen, naproxen and other nonsteroidal anti-inflammatory drugs (NSAIDs) that treat pain and inflammation
- Specific calcium channel blockers to treat high blood pressure
- Specific types of chemotherapy for cancer
- Tricyclics and selective serotonin reuptake inhibitors, which treat depression
What are the symptoms of heart failure?
People can experience heart failure differently. Sometimes symptoms appear suddenly, and sometimes they develop slowly over time.
The most common heart failure symptoms are shortness of breath and swelling in the lower body.
Types of Heart Failure
The main types of heart failure are named for where they occur in the heart:
- Left-sided heart failure
- Right-sided heart failure
- Biventricular heart failure (both sides)
Clinicians also may classify heart failure as:
- Acute: You have active symptoms of heart failure, with either a new diagnosis or with long-term (chronic) heart failure.
- Chronic: You have a history of heart failure, but your condition is relatively stable with no symptoms or with manageable symptoms.
Left-sided heart failure
Left-sided heart failure involves the left ventricle (bottom left chamber of the heart). When the left ventricle doesn’t pump enough blood, it backs up in the blood vessels that carry blood away from the lungs. It’s the most common type of heart failure, and tends to cause breathing symptoms.
Left-sided heart failure can be classified further as heart failure with reduced or preserved ejection fraction:
- In heart failure with preserved ejection fraction (sometimes called diastolic heart failure), the left ventricle can’t relax normally. As a result, the heart can’t fill with blood between beats and things back up.
- In heart failure with reduced ejection fraction (or systolic heart failure), the left ventricle can’t contract (squeeze) normally, so less blood gets into circulation.
Ejection fraction is the percentage of blood the left ventricle of the heart pumps out with every beat. A normal, healthy ejection fraction is 55% to 65%.
Right-sided heart failure
Right-sided heart failure involves the right ventricle (bottom right chamber of the heart). When the right ventricle doesn’t pump well, blood backs up in the blood vessels that carry blood from the rest of the body back to the heart. This can push fluid out of the veins and into other tissue, often leading to swelling.
Biventricular heart failure
Biventricular heart failure is a combination of left-sided and right-sided heart failure. It involves both sides of the heart, and can cause a mix of both types of symptoms.
Acute versus chronic heart failure
Acute heart failure is any heart failure that develops suddenly, such as after a heart attack or with arrhythmia. Chronic heart failure develops over time from medical conditions such as long-term hypertension (high blood pressure) or coronary artery disease.
Congestive heart failure
Many people use the terms heart failure and congestive heart failure interchangeably.
Congestive heart failure involves fluid backing up into the body’s tissues to the point that the tissues get congested and patients have symptoms. The symptoms and complications can become life-threatening, requiring timely medical attention.
How is heart failure diagnosed?
Your health care team may use a variety of strategies and tests to diagnose heart failure.
History and physical exam
A clinician listens to your heart and lungs and measures your blood pressure and weight. They will also ask about your:
- Family’s medical history, especially previous cardiac problems
- Lifestyle (such as whether you smoke or exercise)
- Medications, including prescriptions, over-the-counter drugs and supplements
- Personal medical history
- Symptoms
Blood tests
Blood tests can measure several things related to heart failure:
- Sodium and potassium levels (electrolytes)
- Creatinine, which helps measure how well your kidneys are working
- B-type natriuretic peptide (BNP), a hormone released from the ventricles in response to increased wall tension (stress) that occurs with heart failure
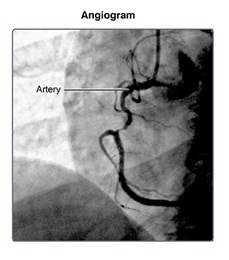
Imaging and other tests
Other tests provide pictures of the heart and surrounding structures or show how well the heart is working:
- Electrocardiogram (EKG or ECG): An electrocardiogram test uses small sensors to measure heart rate (how fast the heart is beating), rhythm (steady or irregular) and electrical impulses.
- Chest X-ray: A chest X-ray is a picture of your lungs, heart and surrounding structures. It can show whether there is fluid in your lungs from heart failure, or if your heart muscle is enlarged.
- Echocardiogram (also called an echo): Echocardiography uses sound waves to create images of your heart. It can show how thick the heart muscle has become, as well as measure ejection fraction.
- MRI: MRI is an advanced imaging test that takes pictures of the heart and surrounding structures. It helps determine your heart function and size and whether there are any changes in the heart muscle. A cardiac MRI may help your doctors identify causes of heart failure.
What are the four stages of heart failure?
There are two classification systems for heart failure, which indicate how severe the condition is. Your doctor might use one or both systems.
NYHA Functional Classification System
The New York Heart Association (NYHA) functional classification considers heart failure symptoms that happen during exercise to determine stage. Patients can go back and forth between stages depending on how well-controlled symptoms are on a given day.
- Stage 1: The person has heart disease, but it isn’t yet causing symptoms or limiting activities.
- Stage 2: The person has mild symptoms that only slightly limit activity.
- Stage 3: The person has significant limitations to activities. He or she is only comfortable when resting.
- Stage 4: The person has major limitations and experiences symptoms when at rest.
ACC/AHA classification system
The American College of Cardiology (ACC) and American Heart Association (AHA) developed a separate system to classify heart failure. Once you reach a specific stage, you remain there or progress, but you do not go backward.
- Stage A: This describes a person who has a high risk of developing heart failure because of family history or personal medical conditions. It’s also called pre-heart failure.
- Stage B: This stage is sometimes called silent heart failure. It means you have changes in your heart function, but you haven’t developed heart failure symptoms yet.
- Stage C: Stage C means heart failure has been diagnosed, and the person has had symptoms.
- Stage D: Stage D is advanced heart failure that isn’t responding to standard treatment. A person usually has symptoms when they are being mildly active or even resting.
How is heart failure treated?
We have many proven treatments to improve heart function, symptoms and survival for patients. Treatments also improve quality of life by:
- Addressing any underlying causes
- Relieving symptoms
- Improving overall health
Education and lifestyle choices
Education is an important part of heart failure treatment. Your team will talk with you about the importance of:
- Controlling blood pressure and controlling blood sugar (if you have diabetes)
- Eating a heart-healthy diet, including controlling sodium
- Participating in moderate exercise
- Recognizing small warning signs in your body, such as swelling or weight gain
- Getting enough sleep
- Losing weight if necessary
- Quitting smoking
- Avoiding alcohol
Medications for heart failure
Certain medications can help treat heart failure and its underlying cause:
- Aldosterone blockers block the effects of the hormone aldosterone, encouraging the body to release sodium and water. They also help prevent scarring in the heart.
- Angiotensin receptor-neprilysin inhibitor (ARNI): Treatment with sacubitril-valsartan reduces excess fluid in the body and relaxes blood vessels. This makes it easier for your heart to pump blood. Alternatives to ARNIs include angiotensin-converting enzyme (ACE) inhibitors andangiotensin receptor blockers (ARBs).
- Beta blockers make the heart beat more slowly and with less force. They also help keep heart rhythm regular.
- Sodium-glucose transport protein 2 (SGLT2) inhibitors are diabetes drugs that have recently been found to be very beneficial in heart failure. They help remove glucose (sugar) via the kidneys into the urine.
Other medications can relieve the heart failure symptoms:
- Diuretics reduce the amount of fluid in the body.
- Vasodilators dilate (open) the blood vessels and reduce the heart’s workload.
- Digoxin helps the heart beat stronger with a more regular rhythm.
- Anti-arrhythmics control arrhythmia and maintain normal heart rhythm.
Surgery for heart failure
Your doctor may recommend surgery to implant a medical device that helps the heart function more effectively:
- Pacemaker, which maintains a steady heart beat in people with a slow or irregular heartbeat
- Implantable cardioverter defibrillator (ICD), which monitors the heart for fast rhythm and delivers an electrical shock to reset normal rhythm
- Left ventricular assist device (LVAD), which takes over the pumping action of the heart
People with advanced heart failure may be candidates for heart transplantation. A heart transplant replaces the diseased heart with a donated heart from a person who has died.
What are the possible complications of heart failure?
Complications of heart failure include:
- Arrhythmia
- Blood clots, which can lead to pulmonary embolism or stroke
- Impaired kidney function or liver function
- Muscle wasting (loss of muscle tissue throughout the body)
- Pulmonary edema (extra fluid in the lungs)
- Respiratory distress
What is heart failure versus heart attack and cardiac arrest?
Heart failure, heart attack and cardiac arrest are different kinds of heart disease. They can be related to each other, but they’re not the same thing.
With heart failure, the heart keeps pumping, just not as effectively. With heart attack (myocardial infarction), blood flow to the heart is blocked, and heart muscle begins to die.
Cardiac arrest means the heart stops beating.