Johns Hopkins Pediatric Moyamoya Center Opens
Multidisciplinary team treating rare disorder includes neurologists, neurosurgeons

The Johns Hopkins Pediatric Moyamoya Center is led by (from left) neurologist Lisa Sun and neurosurgeons Alan Cohen and Risheng Xu.
Johns Hopkins Medicine has launched the first pediatric moyamoya center in Maryland, bringing together a multidisciplinary team to provide specialized care for children with the rare blood vessel disorder.
The effort, led by neurologist Lisa Sun and neurosurgeons Alan Cohen and Risheng Xu, grew organically from years of collaboration and an increasing number of pediatric patients referred to Johns Hopkins for advanced care for the disease. The three physicians also work with colleagues in neuroradiology, anesthesiology, hematology, nursing, child life and the pediatric intensive care unit.
“For any patient with moyamoya, the data shows that care is best at high-volume centers,” Sun says. “So that was a primary impetus for forming a center where we can consolidate treatment and surgery with doctors who have the expertise to do so.”
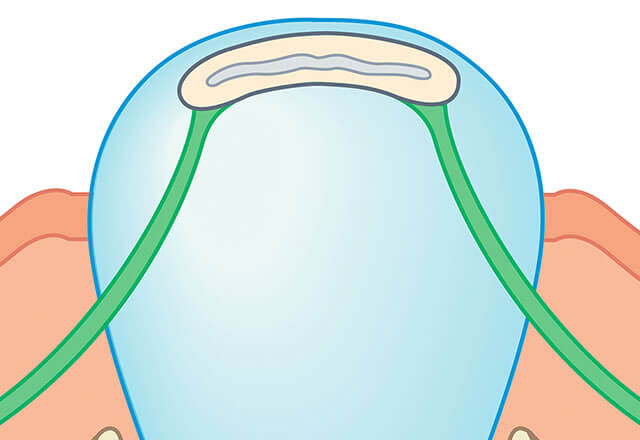
Moyamoya disease is a progressive condition characterized by the narrowing and blockage of the internal carotid arteries, reducing blood flow to the brain and significantly increasing the risk of strokes, hemorrhages and other neurological complications. Most prevalent in East Asia, where it is the leading cause of childhood strokes, moyamoya affects approximately one per 1 million people in the United States.
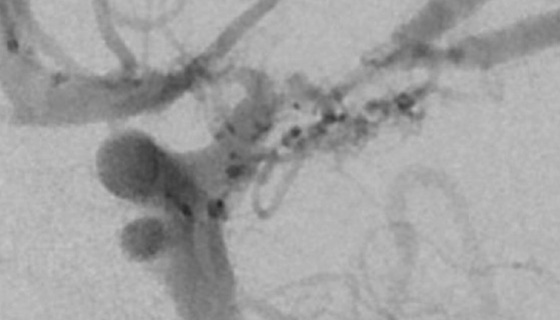
The disease takes its name from the Japanese term for “puff of smoke,” describing the appearance of the fragile, abnormal blood vessels on angiograms.
Johns Hopkins, one of the few medical institutions in the U.S. that specializes in treating moyamoya, has seen more than 100 pediatric patients with the disease since 2003, with the volume increasing in recent years.
Typically, patients first meet with Sun, who performs diagnostic imaging and manages initial treatments, such as antiplatelet and blood pressure therapies. For most patients, revascularization surgery is a critical component of treatment. The process begins with Xu performing a cerebral angiogram — the gold standard for confirming a moyamoya diagnosis and planning surgery. Xu and Cohen then perform the revascularization surgery, which involves connecting healthy scalp blood vessels to the brain to restore blood flow and reduce stroke risk.
“We have a large multidisciplinary team and use a structured neurocritical care pathway,” says Cohen. “Our aim is to help patients navigate safely through the process before, during and after surgery.”
Adds Xu, “The three of us are always talking and consulting each other about each patient and their needs. That type of attention and coordination is very rare.”
Beyond patient care, the physicians at the pediatric moyamoya center are national leaders in research on the disease. Relevant publications include:
“Patient-Reported Outcomes in Childhood Moyamoya Arteriopathy.” Pediatric Neurology, 2025.
“Pediatric Moyamoya Revascularization Perioperative Care: A Modified Delphi Study.” Neurocritical Care, 2024.
“Relative Anemia and Perioperative Stroke in Children with Moyamoya.” Journal of Stroke and Cerebrovascular Disease, 2024.
“Perioperative Management of Pediatric Patients with Moyamoya Arteriopathy.” Journal of Pediatric Intensive Care, 2021.
To refer a patient, call 410-955-7337.
For Clinicians Clinical Connection
Clinicians, discover the latest in research and clinical innovation from Johns Hopkins experts. Access educational videos, articles, CME courses and other resources from our world-renowned institution.
Related Reading
-
Paving a Path for Treating Pediatric Moyamoya
Johns Hopkins neurologist Lisa Sun tackles knowledge gaps in research on the rare blood vessel disorder.
-
Treating Patients with Neurologic Conditions from Prenatal Stages Through Adulthood
In the Johns Hopkins Center for Fetal Therapy and the Greenberg Skeletal Dysplasia Center, multidisciplinary teams of experts provide rare treatments and follow patients throughout their lifetimes.