For a Better Look at High-Grade Glioma, Let's Switch Off the Bright Lights
Neurosurgeon Raj Mukherjee uses fluorescence-guided imaging during operations and researches new ways to apply the approach — all to improve quality of life and outcomes for patients.

Neurosurgeon Raj Mukherjee uses fluorescence-guided imaging during operations and researches new ways to apply the approach — all to improve quality of life and outcomes for patients.
When Johns Hopkins neurosurgeon Raj Mukherjee wants a better look at a patient’s high-grade glioma during brain surgery, he asks a team member to switch off the operating room’s bright lights.
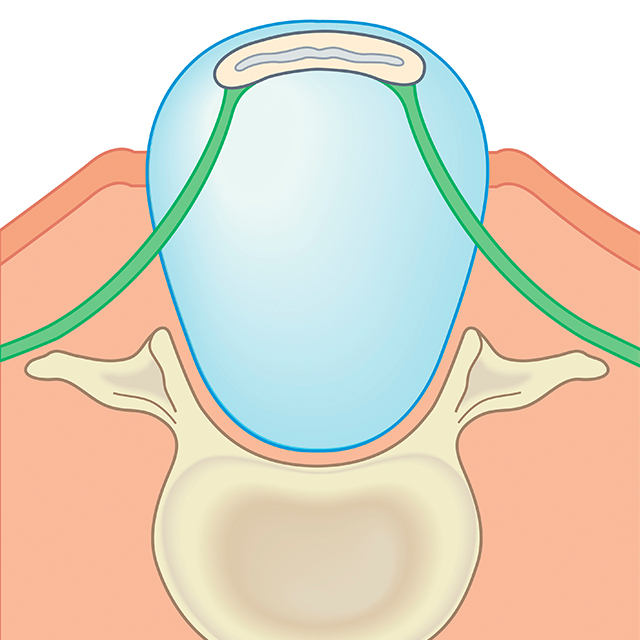
Using a naturally occurring amino acid called 5ALA, which penetrates tumor cell membranes and turns those cells a bright pink under fluorescent blue light, Mukherjee is able to see the glioma in real time. He says anything that helps him differentiate between cancer and healthy tissue is a help.
“Under bright white light, it can be very difficult to see with your naked eye the difference between normal and abnormal brain tissue,” the neurosurgeon says. “I’m happy for any tool we can use to remove more of the cancer without putting the patient’s quality of life at risk.”
Before Mukherjee begins a surgery to remove a high-grade glioma, the patient swallows a small vial of 5ALA, which penetrates the tumor’s cell membranes and lights up in a pink glow when the OR’s bright lights are switched off.
“We shine a blue light on it, and there it is,” he says. “If it’s tumor, it’s hot pink. If it’s normal, it’s dark.”
Mukherjee says fluorescence-assisted surgery can help care teams and patients avoid the need for MRI during surgery.
“That can take a long time,” he says. “And sometimes it’s necessary to get an MRI more than once during surgery. It’s best if we don’t have to keep the patients intubated longer than they need to be. Being able to see the whole tumor in real time during surgery makes everything much easier.”
“Hopkins is focused on maintaining quality of life in patients with brain tumors, rather than just how much cancer we’re able to resect.”
Raj Mukherjee
Exploring New Applications of Fluorescence-Guided Surgery
Florescence-guided surgery offers promise in other areas, says Mukherjee. For now, 5ALA is only FDA-approved for surgery on high-grade gliomas, and is only in use at Johns Hopkins and a few other academic medical centers across the U.S. Researchers at Johns Hopkins and other institutions are working to find ways to use 5ALA and similar fluorescent agents to do more than diagnose cancer.
“There’s something about the molecules we use for florescence that tag tumors, as opposed to normal tissue,” he says. “We’re using it diagnostically now. But if we can attach targeted chemotherapy to those molecules, we’ll have a new treatment modality.”
Mukherjee says clinical research on 5ALA has primarily centered on the extent of resection. But researchers at Johns Hopkins are looking beyond that.
“We’re trying to expand the way we think of patient-centered quality,” he says. “Hopkins is focused on maintaining quality of life in patients with brain tumors, rather than just how much cancer we’re able to resect.”
Because high-grade gliomas can invade between healthy cells, they can be difficult to remove without harming healthy brain tissue. Mukherjee calls the ability to light up tumor cells “a game changer.”
“It fundamentally changes how we do surgery,” he says. “For someone who has a glioblastoma, anything you can do to give people more time is deeply, deeply meaningful. This is one of those things. It’s wonderful to be able to leave an operating room and tell families with confidence that we got it all.
“That’s a great relief to the patient, the family and the surgeon.”
To refer a patient, call 410-955-6406.
For Clinicians Clinical Connection
Clinicians, discover the latest in research and clinical innovation from Johns Hopkins experts. Access educational videos, articles, CME courses and other resources from our world-renowned institution.
Related Reading
-
Treating Patients With Complex Brain Tumors
Neurosurgeon Youssef Comair specializes in craniotomies to remove falcotentorial meningiomas.

-
Treating Patients with Neurologic Conditions from Prenatal Stages Through Adulthood
In the Johns Hopkins Center for Fetal Therapy and the Greenberg Skeletal Dysplasia Center, multidisciplinary teams of experts provide rare treatments and follow patients throughout their lifetimes.