Electrophysiologists Use Novel Device in Patients with Irregular Heart Rhythms
Charles Love, director of the Johns Hopkins Cardiac Rhythm Device Service, discusses the EV-ICD, which can yield considerable benefits for those who require care.

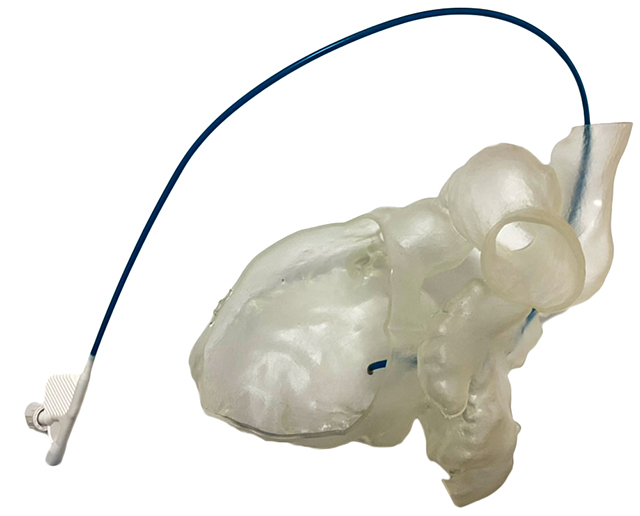
A new device for patients with irregular heart rhythms, an extravascular implantable cardioverter-defibrillator (EV-ICD), is pictured on X-ray. The device is placed to the left side of the chest with the wire outside the vascular space, eliminating the need to thread wires through blood vessels.
While electrophysiologists at Johns Hopkins use a range of devices for patients with irregular heart rhythms, one of the newest is an extravascular implantable cardioverter-defibrillator (EV-ICD), which experts place to the left side of the chest with the wire outside the vascular space — eliminating the need to thread wires through blood vessels.
This apparatus constantly monitors heart rhythm and responds within seconds, either delivering pacing pulses to the heart to terminate the arrhythmia or delivering a lifesaving shock, explains electrophysiologist Charles Love, director of the Johns Hopkins Cardiac Rhythm Device Service. This defibrillator has just one wire that goes under the sternum to protect against sudden cardiac death in the event of ventricular tachycardia.
“I tell patients it’s like having your own paramedic watching and walking around with you, waiting to see your heart go out of rhythm,” Love says. “Before you can dial 911, it has charged up and saved your life.”
In the U.S., Love and his team are among few physicians trained to use this technology that brings several advantages. First, the wire sits under the sternum, much closer to the heart than the wire for a subcutaneous ICD, which goes above the sternum. Therefore, he says, it doesn’t require as much energy to restore a normal heart rhythm. This, in turn, allows the apparatus to be much smaller than its predecessors. In many cases, it delivers pulses of sufficient strength to help pace the heart out of bad rhythms instead of providing a full-on shock. The tool thus preserves its own power and — because of its size and placement — is more comfortable for patients over time.
“I tell patients it’s like having your own paramedic watching and walking around with you, waiting to see your heart go out of rhythm. Before you can dial 911, it has charged up and saved your life.”
Charles Love
The EV-ICD is appropriate for people who have a familial risk of sudden cardiac arrest and conditions such as long QT syndrome, Brugada syndrome and hypertrophic cardiomyopathy, says Love. It’s best for individuals who need only occasional pacing, such as younger, active adults; swimmers, weightlifters and others who use their upper body frequently; and people with an artificial heart valve. The device collects information about heart events and its performance, and transmits that wirelessly to a bedside monitor or cell phone app — then to a server checked daily by the cardiologist’s office.
Following an outpatient procedure to place the device — which is functional after implanted for about 12 years — patients generally stay in the hospital one night for pain management, Love says. He and colleague Andreas Barth have implanted about 30 of the devices since the beginning of this year.
“Patients tend to have a little bit more pain from this implantation than from some other devices, because we push our finger up underneath the diaphragm muscle to place the wire,” Love says. The good news? The wire is located in an area of the chest that doesn’t bend and flex much, and it’s much less likely to fracture like transvenous wires associated with some other devices, he says. In addition, should the wire need to be removed, the process is much easier and safer than that for wires that are located inside the blood vessels or heart. Patients are followed annually for checkups from there, he says.
To refer a patient, call 443-997-0270.
For Clinicians Clinical Connection
Clinicians, discover the latest in research and clinical innovation from Johns Hopkins experts. Access educational videos, articles, CME courses and other resources from our world-renowned institution.
Related Reading
-
Caring for Patients with Arterial Disease
Vascular surgeon Rebecca Marmor partners with referring physicians to help patients address peripheral arterial disease, aortic aneurysms, carotid disease and dialysis access.
-
Creative Approaches for Patients with Congenital Heart Disease and Electrical Heart Complications
Konstantinos Aronis shares insight into how he and his team care for this unique set of patients.