New Gene Therapy for Duchenne Muscular Dystrophy
Novel treatment may help young boys with degenerative muscle disease stay ambulatory for longer.

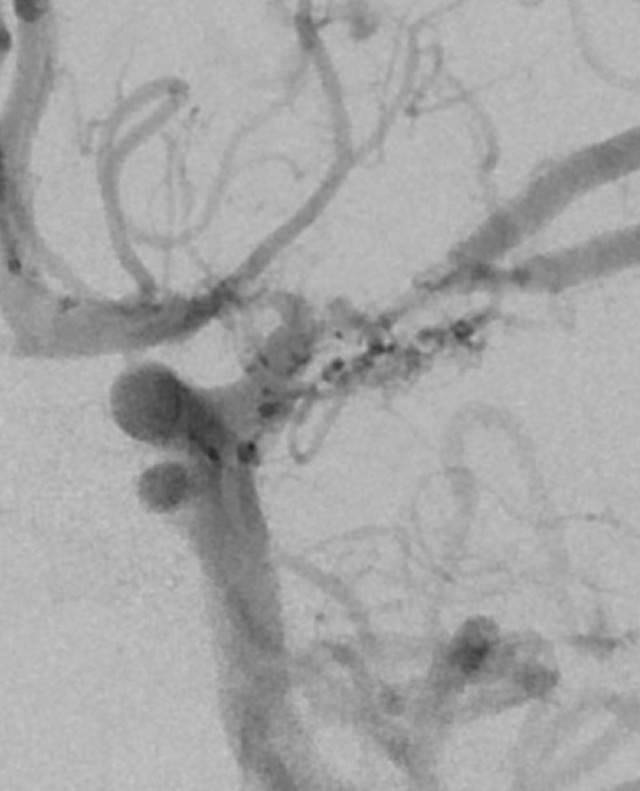
A muscle biopsy in early-stage Duchenne muscular dystrophy shows diffuse muscle fiber degeneration and the replacement of healthy muscle with fibrosis and fatty tissue.
Patients with Duchenne muscular dystrophy (DMD) have long been without effective treatment options. Longstanding treatments such as corticosteroids and exon-skipping therapies can prolong the time it takes for the disease’s devastating symptoms to manifest, but neither address DMD’s underlying cause — the body’s inability to produce the protein dystrophin.
The degenerative muscle disorder is caused by deletions, duplications, point mutations and premature stop codons in the gene that makes dystrophin, which stabilizes muscle cell membranes and supports the contractile apparatus. Without dystrophin, muscle becomes fragile and easily degenerates.
A new single-dose intravenous gene therapy, delandistrogene moxeparvovec, creates “micro-dystrophin” — a scaled-down version of the large gene that encodes dystrophin — and targets the skeletal and heart muscles. A trial showed statistically significant improvement in the expression of dystrophin and improvement in motor function in 4- and 5-year-olds, and the drug has since been approved for all patients ages 4 and up who have a confirmed mutation in the DMD gene.
“This is a disease that is relentlessly progressive, and uniformly fatal at a younger age,” says Johns Hopkins neurologist Jessica Nance. “So, it’s exciting to have identified a therapy with the potential to significantly impact the course of the disease. It’s not a panacea, but it’s at least something that can help us improve the quality of life for these boys.”
Johns Hopkins treated its first patient with the new therapy in July. Nance and her colleagues are building a gene therapy treatment team to monitor patients for 12 weeks after their infusion based on a detailed protocol they designed, as well as a prior authorization team to help patients and their families navigate insurance coverage.
“This is an extremely advanced therapy,” Nance says, “and our team is poised to work through all of the red tape that it takes to get this drug approved and delivered for our patients.”
“It’s exciting to have identified a therapy with the potential to significantly impact the course of the disease.”
Jessica Nance
DMD mostly affects boys and occurs in 1 in 3,500 to 5,000 male newborns, generally causing immobility by ages 10–12, cardiomyopathy due to weakened heart muscles, and early death. Without dystrophin, boys with the X-linked condition suffer from muscle scarring, inflammation in muscles and eventually atrophy or reduced muscle mass.
The hope is that the drug will lead to longer ambulation.
“This new therapy is a big deal,” says neurologist Tom Crawford, Nance’s colleague at the pediatric neuromuscular clinic. “But because it is so new, there remains a lot we don’t yet know about who will most benefit, and for how long. Still, the potential for a one-time gene transfer therapy is real.”
Boys who receive the treatment can experience a variety of side effects due to their bodies receiving millions of viral particles and having dystrophin for the first time. After their infusion, patients will have weekly doctor’s visits and bloodwork during the monitoring period. Liver function tests can become abnormal, and patients may develop hepatitis, requiring inpatient treatment. The drug can also cause inflammation and possibly myocarditis, so patients are put on extra corticosteroids during the monitoring period. Doctors will track platelet levels, as thrombocytopenia can occur, and patients may experience rhabdomyolosis or myositis. Nance and her team will monitor creatine kinase levels to make sure there are no negative changes in muscle function.
The gene therapy team includes pharmacists who have the expertise to receive, store and prepare the drug, a group of prescribing physicians who treat patients with DMD, as well as subspecialists available to treat potential side effects.
Between The Johns Hopkins Hospital and the Kennedy Krieger Institute, which also sees patients with DMD, Nance estimates that there are nearly 90 eligible patients.
Nance is principal investigator for the Johns Hopkins site for the EMBARK study, which is continuing to test the drug’s efficacy. The current trial is a two-year double-blind, placebo-controlled study with 4- to 7-year-olds, now in its second year. Patients will be followed for five years.
“We have really been waiting for something like this for a long time,” Nance says. “I think this is a new frontier in therapy. It’s just going to keep getting better for these kids.”
To refer a patient to pediatric neurology, call 410-955-4259.
For Clinicians Clinical Connection
Clinicians, discover the latest in research and clinical innovation from Johns Hopkins experts. Access educational videos, articles, CME courses and other resources from our world-renowned institution.
Related Reading
-
Treating Patients with Neurologic Conditions from Prenatal Stages Through Adulthood
In the Johns Hopkins Center for Fetal Therapy and the Greenberg Skeletal Dysplasia Center, multidisciplinary teams of experts provide rare treatments and follow patients throughout their lifetimes.
-
Paving a Path for Treating Pediatric Moyamoya
Johns Hopkins neurologist Lisa Sun tackles knowledge gaps in research on the rare blood vessel disorder.