Treating Patients with Neurologic Conditions from Prenatal Stages Through Adulthood
In the Johns Hopkins Center for Fetal Therapy and the Greenberg Skeletal Dysplasia Center, multidisciplinary teams of experts provide rare treatments and follow patients throughout their lifetimes.

A digital illustration shows myelomeningocele, the most severe form of spina bifida.
For patients with congenital conditions such as skeletal dysplasia and spina bifida, Johns Hopkins clinicians and physicians offer cutting-edge methods and uncommon transitional care models.
Pediatric neurosurgeon Mari Groves, who specializes in spina bifida, treats her patients prenatally and into adulthood. Within the Johns Hopkins Center for Fetal Therapy, she performs minimally invasive fetoscopic repair of myelomeningocele — a procedure provided at fewer than 10 centers in the U.S. (See sidebar.) As part of the Greenberg Skeletal Dysplasia Center, Groves also follows patients from the nascent phases of life into maturity. The center is one of the few in the country that does so.
“Because I care for my patients across the span of their lives,” she says. “I have a somewhat unique perspective. It helps me counsel my prenatal patients and even my pediatric patients, and it allows me to deeply consider disease processes.”
The Greenberg Center, the roots of which date to the 1950s, offers multidisciplinary care from nationally recognized experts, such as Director Julie Hoover-Fong, who is the current chair of the medical advisory board of Little People of America. The center’s team is made up of clinicians from prenatal genetics, maternal-fetal medicine, gynecology and obstetrics, ophthalmology, orthopaedics, otolaryngology and pulmonology. In the summer of 2024, the Greenberg Center partnered with Little People of America to host the organization’s national conference in Baltimore. Groves presented.
“Because I care for patients across the span of their lives, I am better able to counsel my prenatal patients and my pediatric patients, and it allows me to deeply consider disease processes.”
Mari Groves
Groves and colleagues additionally collaborate with the Kennedy Krieger Institute’s Center for Spina Bifida and Related Conditions — directed by physical medicine and rehabilitation physician Sarah Korth. Korth is an attending physician at both The Johns Hopkins Hospital and the institute. This center brings together occupational therapy, physical medicine and rehabilitation, social work, orthopaedics, physical therapy, neuropsychology and nutrition for individualized care. Having such a team allows clinicians to be aggressive with identifying patients’ needs early in their lives, Groves says. This may include developing approaches for bowel and bladder issues, as well as lack of leg strength.
“We’re entering an age now, especially with the advent of better technology, when we’re seeing more and more patients with these congenital disorders living into adulthood,” Groves says. “We’re really at the forefront of care for these patients.”
To refer a patient to pediatric neurosurgery, call 410-955-7337.
The Benefits of Fetoscopic Repair for Myelomeningocele
At the Johns Hopkins Center for Fetal Therapy, neurosurgeon Mari Groves performs both fetoscopic and open repair for myelomeningocele — the most severe form of spina bifida. According to the Management of Myelomeningocele Study, which was published in 2011, benefits of prenatal surgery for spina bifida include:
- a more than 50% reduction in the need for shunting treatment for hydrocephalus
- an almost tenfold reduction in the development of secondary neurological conditions
- better spinal cord function
While both fetoscopic and open methods offer significant benefits to the baby, Groves says, the mother can have complications with future pregnancies from the open method. Considerations such as this are why she and the fetal therapy team consult with families and present all options.
“Often, we’re meeting families for the first time after they’ve just received incredibly devastating information,” she says. “Our role is to show them what opportunities there are, and support them with the medical facts to make the best decision for them.”
For Clinicians Clinical Connection
Clinicians, discover the latest in research and clinical innovation from Johns Hopkins experts. Access educational videos, articles, CME courses and other resources from our world-renowned institution.
Related Reading
-
Better Understanding of Chiari Malformation
Johns Hopkins’ participation in the Chiari Surgical Success Scale and a similar study for nonsurgical patients could help doctors make better treatment decisions.
-
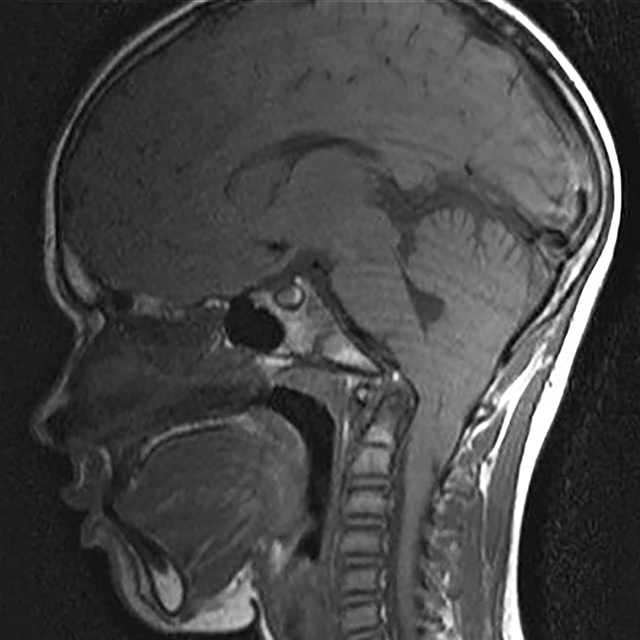
New Research Illuminates How Ultrasound Could Be Used in Fight Against Glioblastoma and Other Brain Conditions
Johns Hopkins neurosurgeons are among the first in the U.S. to use magnetic resonance guided focused ultrasound, also known as MRgFUS, to investigate how it may be applied to ablate diseased tissue and traverse the blood-brain barrier.