Proton Therapy Case Studies – Gynecologic Cancers
Proton beam radiation therapy is an FDA-approved treatment modality. Proton beam therapy directs a beam of protons (positively charged subatomic particles) at the radiation target, where they deposit the bulk of their energy in the last few millimeters of their range; tissue beyond the tumor receives very little radiation dose because of the absence of exit dose. Given the physical characteristics of protons (no exit dose), proton beam therapy helps save vital organs that are close to the tumor.
Case 1: Uterine Carcinosarcoma With Extended Fields to Para-Aortic Nodes
Patient is a 60-year-old woman with postmenopausal woman with a history of FIGO stage IIIC1 (grade 3 carcinosarcoma of the uterus, 75% myometrial invasion (MMI), no lymphovsacular space invasion (LVSI), 2/2 lymph nodes involved. She was treated with total abdominal hysterectomy and bilateral salpingo-oopherectomy with pelvic lymph node dissection and 6 cycles of adjuvant Carbo/Taxol.
Treatment: Given her high grade and aggressive histology, decision was made to use the extended field to cover para-aortic nodes. She was treated with 55 Gy (45 Gy pelvis + 10 Gy boost)

Radiation Field
Case 2: Recurrent Endometrial Cancer in Paraaortic Node
Patient Case
Patient is a 76-year-old woman with a hx of breast ca and stage IIIC1 high grade uterine carcinosarcoma initially diagnosed in 2013 treated with total abdominal hysterectomy, bilateral salpingo-oopherectomy, and lymph node dissection. Pathology demonstrated <50% myometrial invasion, lymphovascular space invasion and evidence of 6/6 involved right pelvic lymph nodes and 2/5 involved left pelvic lymph nodes). She went on to receive 6 cycles of chemotherapy followed by external beam radiation with intensity modulated radiation therapy (IMRT) to 45 Gy and vaginal brachytherapy 7 Gy x 3. She then had a biopsy proven recurrence in a para-aortic node 4 years later.
Treatment
She was treated with proton therapy due to prior radiation to reduce dose to organs at risk.
Reason for protons: Prior radiation therapy – reduced dose to organs at risk.
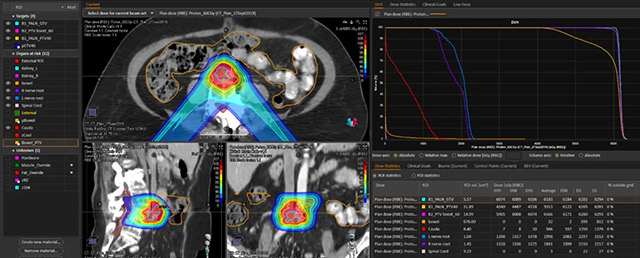
Proton Plan: Isodose, Dose volume histogram, Dose Statistic

Proton Plan: Clinical Goal

Proton Plan Vs Photon Plan: DVH

Proton Plan Vs Photon Plan: Clinical Goal
Case 3: Re-Irradiation in the Setting of Metastatic Cervical Cancer to Enlarging Lymph Node
A 63 year old woman presented with squamous cell carcinoma of the cervix that was metastatic to the para-aortic and pelvic lymph nodes. She completed chemoradiation with external beam to 45 Gy with a pelvic boost to 65 Gy along with weekly cisplatin. This was followed by a brachytherapy boost to the cervix, 700cGy in 1 fraction. She then had five cycles of adjuvant chemotherapy with carboplatin/paclitaxel. She returned to clinic with biopsy proven recurrent disease in an enlarging left iliac node two years later, compressing the obturator nerve. She was started with carboplatin/taxol/avastin.
Radiation Treatment
She received proton therapy in order to minimize dose to organs at risk (OARs). The patient had already showed signs of radiation toxicity with sacral insufficiency. Thus, proton radiation would be able to minimize additional dose to OARs including sacral nerves and bowel.

Proton vs Photon Plan Comparison

Organs at Risk Constraints
In this case, due to the lymph node pressure on the obturator nerve and the patient’s developing symptoms, obturator sparing using proton therapy was advantageous. Using a three beam technique.

Case 4: Recurrent Endometrial Cancer in Prior Port Sites
Patient is a 60 y.o. post-menopausal woman with a history of FIGO Stage IB (Grade 1) endometrioid endometrial carcinoma s/p total laparoscopic hysterectomy/bilateral salpingo-oopherectomy and sentinel lymph node dissection. Pathology was significant for 76% myometrial invasion, no lymphovascular space invasion, negative margins, hormone positive with concern for isolated tumor cells vs benign mesothelial cells on ultra-staging for the bilateral sentinel lymph nodes. She then received adjuvant external beam radiation (45 Gy in 25 fractions) to the pelvis and high dose rate brachytherapy to the vaginal cuff (10 Gy in 2 fractions) because of high-risk features including isolated tumor cells, and loss of mismatch repair proteins. She presented with recurrence two years later, in two port sites, one in each the right and left abdomen. She underwent resection of both nodules.
Treatment
Protons were used for boost after initial photon plan: Right side was treated with 45 Gy + 19.8 Gy; Left side 45 Gy + 14.4 Gy. The use of protons allowed for additional sparing of bowel dose to reduce toxicity due to her prior radiation.

Boost Plan

Composite: Original External Beam
Radiation/Brachy + Port Recurrence Plan
Case 5: Prior Radiation for Colorectal Cancer, New Diagnosis of Serious Carcinoma
Patient is a 76-year-old woman with a history of colorectal cancer s/p chemoradiation in 2007 (records unavailable) and FIGO stage IIIC1 uterine serous carcinoma treated with hysterectomy and bilateral salpingo-oopherectomy two years prior. Pathology demonstrated >50% myometrial invasion, lymphovascular space invasion and, cervical stromal invasion. Additionally, 1 out of 6 lymph nodes were involved in the right obturator chain. She received 6 cycles of adjuvant carboplatin/paclitaxel.
Treatment
She received proton therapy due to her prior radiation for her colorectal cancer in 2007. She was treated with 4000cGy in 20 fractions to the pelvic lymph nodes alone with 2400cGy x 6 fractions vaginal cylinder brachytherapy to the full vaginal length.
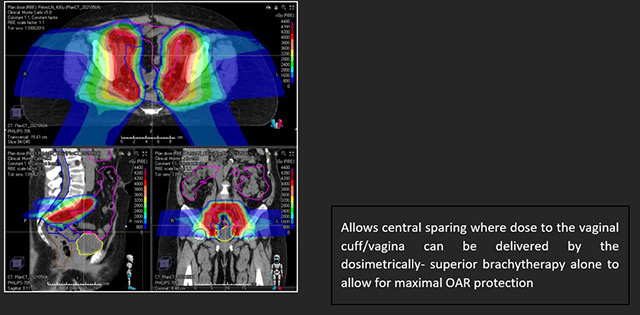
Reason for protons: Prior Radiation
Radiation Field

Radiation Fields
Case 6: Prior History of Colorectal Cancer With Ostomy, Newly Diagnosed Endometrial Cancer
Patient is a 74-year-old woman with a history of multifocal colorectal cancer managed with near-total proctocolectomy (permanent ostomy) with adjuvant chemoradiation to 50.4Gy in 2001 (records unavailable) and a remote supracervical hysterectomy. She presented twenty years later with a 4cm localized endometrioid adenocarcinoma at the vaginal apex.
Treatment
Given her prior radiation plan, proton therapy was recommended to minimize dose to organs at risk. She was treated with an SIB plan (SIB is simultaneous integrated boost, so a smaller volume will get a higher dose per fraction). The pelvic lymph nodes, vagina, parametrium, and ovaries received 40 Gy, the inguinal lymph nodes received 44 Gy, and the gross residual disease at the vaginal apex received 50 Gy. Using protons, we were able to dose escalate in the definitive treatment setting while protecting small bowel as well as the ostomy.

Radiation Fields

Great ostomy/stoma sparing!
Proton Therapy Gynecologic Experts
Akila Viswanathan, MD MPH
- Director, Johns Hopkins Radiation Oncology and Molecular Radiation Sciences
Expertise: Radiation Oncology
