Treatments and Procedures: Epilepsy Surgery
With so many options for treatment, surgery for epilepsy is no longer considered a last resort. Epilepsy surgery may be able to offer relief when medications either cannot control seizures or cause unmanageable side effects.
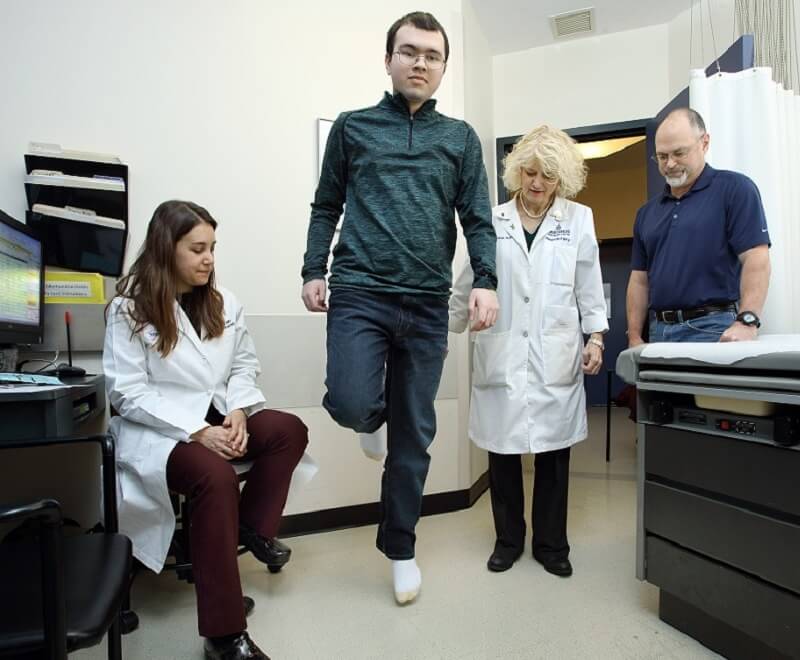
Johns Hopkins epilepsy experts are skilled in a range of surgical procedures that can help bring seizures under control, including less invasive techniques.
Epilepsy Surgery: Why Choose Johns Hopkins
- Working together, our team of neurologists and neurosurgeons offers a highly individualized approach to determining the best surgical treatment for each patient, regardless of age or severity of the epilepsy.
- Our neurosurgeons are exceptionally experienced in all currently used surgical procedures to address even the most challenging seizures.
- We have access to advanced technologies to pinpoint seizure-causing areas in the brain and address them with precision.
- Clear, expert guidance from our professionals helps you fully understand the process, potential risks and benefits of any epilepsy surgery procedure.
Epilepsy Surgery: What to Expect
Your doctor may discuss surgical options with you if you or your child is having seizures that are frequent or difficult to control despite treatment with at least two anti-seizure medications.
The type of epilepsy surgery the doctor recommends depends on where the seizures start in the brain and what type of seizures you or your child is experiencing.
Surgery to Diagnose Epilepsy
Before recommending a particular treatment, your doctor will need to identify where in the brain your seizures originate. Some diagnostic procedures for epilepsy involve surgery:
- Depth electrodes are tiny probes surgically implanted through small holes in the skull and brain covering that can monitor electrical activity.
- Subdural strips and grids are groups of electrodes arranged in strips or sheets. A surgeon places them inside the skull through a surgical opening called a craniotomy.
- Brain mapping is sending a small amount of electrical current through electrodes to identify important functional areas of the brain. This process can help surgeons address the focus of seizures while avoiding these essential areas.
Robotic-assisted stereoelectroencephalography (sEEG) is a less-invasive alternative to craniotomy. Where craniotomy involves removing an entire piece of skull, robotic sEEG requires only tiny holes, through which small electrodes are placed. These individual electrodes aren’t as bulky as subdural strips and grids, so doctors can better access delicate, hard-to-reach spots of the brain with greater precision.
Surgical Procedures to Control Seizures
- Laser interstitial thermal therapy (LiTT) or laser ablation is a minimally invasive procedure that uses computer navigation to target and destroy the seizure-causing lesion.
- Focal resection is the surgical removal of a lesion, such as a scar or growth, from the brain through a craniotomy, a temporary opening in the skull.
- Vagus nerve stimulation (VNS) and responsive neuro-stimulation (RNS) uses a surgically implanted device to interrupt disorganized electrical signals that bring on seizures.
- Corpus callosotomy prevents the spread of seizures across the fibrous channel that connects the left and right halves (hemispheres) of the brain.
- Hemispherectomy is a surgical removal of extensive damage or malformation that involve half (hemisphere) of the brain. Hemispherectomy is usually done in children with severe seizures.
Patient Resources
A new diagnosis of seizures in a child brings up many questions for parents, families and caregivers. If Your Child Has Seizures: A Guide for the Parents, Families, and Caregivers of Newly Diagnosed Children with Epilepsy or a Seizure Disorder can help you get up to speed quickly on what to expect and how to get help and support.