Johns Hopkins Pediatric Transport has been serving Maryland’s children, families and front-line community hospitals since 1992. We provide the highest quality, compassionate care to our region’s sickest and most severely injured young patients.
Our pediatric critical care team is available 24/7 to transport children who need care at Johns Hopkins Children’s Center and other medical facilities. During transport, we may also use telemedicine through audio and/or video telecommunication systems.
Who and How We Transport
Our team arranges transport for approximately 3,500 infants, children, adolescents and young adults each year from more than 60 regional health-care facilities, as well as from national and international centers.
Among the transported patients we help are:
- Children in cardiac arrest or other cardiac emergencies
- Trauma and burn victims
- Children with life-threatening neurosurgical emergencies
We have experience with ground, helicopter and fixed-wing transports of children who require advanced modes of respiratory support, including:
- Noninvasive positive pressure with high-flow nasal cannula or bilevel positive airway pressure (BiPAP)
- Conventional mechanical ventilation
- Inhaled nitric oxide
- High-frequency oscillation
We also offer transport for those who need extensive hemodynamic support, including patients on vasopressor infusions or ECMO.
Requests for Transport
For consultations or transfer requests, contact the Hopkins Access Line at 410-955-9444.
-
All pediatric transfer requests are received by a pediatric critical care transport nurse. From there, the nurse:
- Triages the transfer referral call
- Provides recommendations based on established medical protocols
- Communicates with the sending and receiving providers, including any needed consulting services
- Determines the need for specialty care, coordinating the transport process from team dispatch to patient retrieval, using our patient transport triage tool
Pediatric critical care and emergency medicine physicians help provide advice regarding medical management for patients even before our team arrives at the referring institution, as well as during transport.
-
-
For follow-up on patient referrals, contact Bruce Klein or Corina Noje.
More About Johns Hopkins Pediatric Transport
-
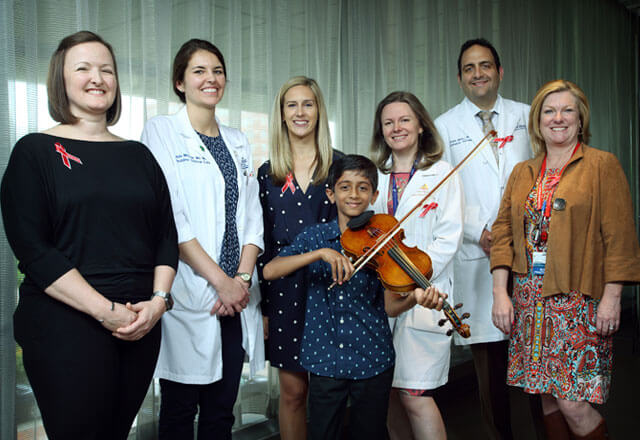
Meet Our Team
Our team of experts includes highly-trained EMS clinicians, pediatric critical care nurses and transport professionals.
-
Our Research
We continuously aim to improve outcomes of our most critically ill or injured patients, through staff education, innovation, and research to ensure maximal safety during transport.
Frequently Asked Questions
-
Depending on numerous factors, your child will either be transported by ambulance or helicopter. A few deciding factors include stability of your child, distance and weather.
-
Most patients will be brought into the pediatric emergency room, and then your child will be assessed for bed placement. However, some patients will be directly admitted to our pediatric intensive care unit, pediatric cardiac intensive care unit, or to our pediatric floors. Patients’ conditions often change, and sometimes where they are admitted changes to best meet the needs of your child.
-
If the patient is being transferred by ground, one parent or guardian can accompany your child while riding in the front seat of the ambulance. If being transported by air, we try our best; however, unfortunately, depending on team configuration and total weight, this is not always possible.
-
Depending on the severity of your child’s condition, they may or may not be admitted to the hospital following their workup in the emergency room. Knowing this is a possibility, please be sure you have means of transportation available. The transport team will not be able to take you home after your child is evaluated.
Featured Stories
-
PICU ‘Superheroes’ Come to Harrison’s Rescue
"Superheroes landed on the roof and saved my son’s life.” That’s how Mike Carter describes the lifesaving event that saved his 6-year-old son, Harrison.

-
Telemedicine: Improving Brain Injury Outcomes
After three-year-old Timothy fell headfirst off his bed onto the hardwood floor, his pediatrician recommended imaging at the nearest emergency department.

-
Honoring Trauma Patients
Whether a motorcycle accident or another complex and often life-threatening injury, trauma providers are greatly challenged in caring for patients facing a serious trauma injury.