Femur Fracture Open Reduction and Internal Fixation
What is a femur fracture open reduction and internal fixation?
Open reduction and internal fixation (ORIF) is surgery used to stabilize and heal a broken bone. You might need this procedure to treat your broken thighbone (femur).
The femur is the large bone in the upper part of your leg. Different kinds of trauma can damage this bone, causing it to fracture into 2 or more pieces. This might happen to the part of the femur near your knee, near the middle of the femur, or in the part of the femur that forms part of your hip joint. In certain types of femur fractures, your femur has broken, but its pieces still line up correctly. In other types of fractures (displaced fractures), the trauma moves the bone fragments out of alignment.
If you fracture your femur, you usually need ORIF to bring your bones back into place and help them heal. During an open reduction, orthopedic surgeons reposition your bone pieces during surgery, so that they are back in their proper alignment. This contrasts with a closed reduction, in which a healthcare provider physically moves your bones back into place without surgically exposing your bone.
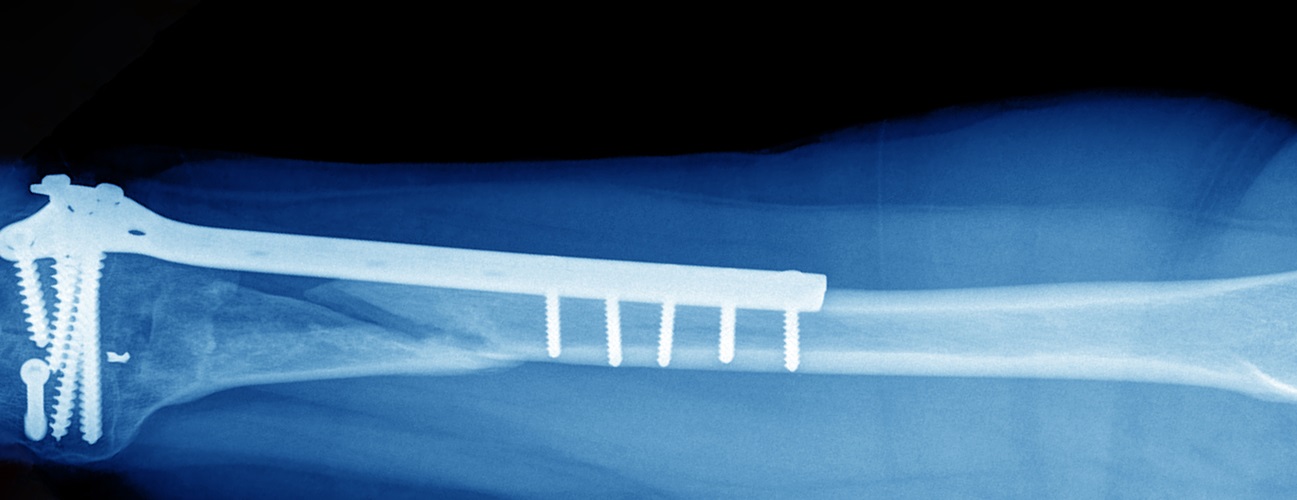
Internal fixation refers to the method of physically reconnecting your bones. This might involve special screws, plates, rods, wires, or nails that your surgeon places inside your bones to fix them in the correct place. This prevents your bones from healing abnormally. For a fracture in the long, middle part of your femur, your surgeon may insert a long metal rod through the middle of your bone. The entire operation usually takes place while you are asleep under general anesthesia.
Why might I need a femur fracture open reduction and internal fixation?
Certain medical conditions may make fracturing your femur more likely. For example, if you are an older adult, osteoporosis increases your risk for fracturing your femur. Your femur might also be more likely to break if you have bone cancer. Motor vehicle accidents, sports-related injuries, gunshot injuries, and falls are common sources of trauma that can lead to a femur fracture. A direct blow to your hip may break the part of the femur associated with your hip joint.
Most people with a fractured femur need some sort of surgery, usually ORIF. Without the surgery, your broken femur may not heal properly. ORIF can place your bones back into their proper configuration. This significantly increases the chance that your bone will heal properly. Your healthcare provider might recommend nonsurgical treatment for a very young child, or for people with other medical conditions that make surgery more dangerous.
You might need ORIF for a fracture that occurs anywhere along your femur, including the portion that forms part of your hip joint. In a “broken hip,” it is actually part of your femur that breaks, and not part of the hipbone itself.
What are the risks for femur fracture open reduction and internal fixation?
Most people do very well after ORIF for their femur fracture. However, rare complications can sometimes occur. Possible complications include:
- Infection
- Bleeding
- Nerve damage
- Blood clots
- Fat embolism
- Healing of the fractured bone in an abnormal alignment
- Irritation of the overlying tissue from the hardware
- Complications from anesthesia
There is also a risk that the fracture won’t heal properly and that you’ll need repeat surgery.
Your risk for complications may vary according to your age, the anatomy of your femur fracture, and other medical conditions. For example, people with low bone mass or diabetes may be at greater risk for some complications. Smokers may also have an increased risk. Ask your healthcare provider about the risks that most apply to you.
How do I get ready for a femur fracture open reduction and internal fixation?
ORIF often takes place as an emergency or urgent procedure. Before your procedure, a healthcare provider will take your medical history and do a physical exam. You’ll need imaging of your femur, probably with an X-ray or computed tomography scan (CT). Tell your healthcare provider about all the medicines you take, including over-the-counter medicines like aspirin. Also, let him or her know the last time you ate.
In some cases, your healthcare provider might do your ORIF as a planned procedure. If so, you might need to have your leg placed in traction while you wait for surgery. Talk with your healthcare provider about how you can prepare for the surgery. Ask whether you should stop taking any medicines ahead of time, like blood thinners. You’ll need to avoid food and drink after midnight the night before your procedure.
What happens during a femur fracture open reduction and internal fixation?
Your healthcare provider can help explain the details of your particular surgery. These details will depend on the location and severity of your injury. An orthopedic surgeon and a team of specialized healthcare professionals will do the surgery. The whole operation may take a few hours. In general, you can expect the following:
- You will receive general anesthesia to make you sleep through the operation, so that you won’t feel any pain or discomfort during the procedure. (Or, you may receive local anesthesia and a medicine to help you relax.)
- A healthcare provider will carefully monitor your vital signs, like your heart rate and blood pressure, during the operation. You may have a breathing tube inserted down your throat during the operation to help you breathe.
- After cleaning the affected area, your surgeon will make an incision through your skin and muscle of your thigh.
- Your surgeon will bring the pieces of your femur back into alignment (reduction).
- Next, your surgeon will secure the pieces of your femur to each other (fixation). To do this, he or she may use screws, metal plates, wires, or pins. For a fracture in the middle part of your femur, surgeons often use a specially designed long metal rod that passes through the middle of the bone. It screws into the bone at both ends. (Ask what your surgeon will use in your case.)
- Your healthcare provider may make other repairs, if necessary.
- After the team has secured your bone, the layers of skin and muscle around your thigh will be surgically closed.
What happens after a femur fracture open reduction and internal fixation?
Talk to your healthcare provider about what you can expect after your surgery. You may have significant pain after your procedure, but pain medicine may help ease your pain. You should be able to resume your normal diet fairly quickly. You will probably have imaging procedure done, like an X-ray, make sure your surgery was successful. Depending on the extent of your injury and your other medical conditions, you might be able to go home within the next couple of days.
Talk with your healthcare provider about how you can move your leg and whether it’s OK to put weight on it. This will depend on the type of injury you have. You may need to protect your leg from water. Follow all your healthcare provider’s instructions carefully. You might need to take a medicine to prevent blood clots (a blood thinner) for a little while after your surgery. Your healthcare provider might not want you to take certain over-the-counter medicines for pain. Some of these can interfere with bone healing. Your healthcare provider may advise you to eat a diet high in calcium and vitamin D as your bone heals.
You might have some fluid draining from your incision. This is normal. Let your healthcare provider know right away if you see an increase in redness, swelling, or draining from your incision, a high fever, chills, or severe pain. Also, let him or her know about any loss of feeling in your leg.
Make sure to keep all of your follow-up appointments. You may need to have your stitches or staples removed a week or so after your surgery.
At some point, you may need physical therapy to restore strength and flexibility to your muscles. Doing your exercises as prescribed can improve your chances for a full recovery. Most femoral fractures take about 4 to 6 months to heal completely, but you should be able to resume many activities before this time.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure





.png?h=170&iar=0&mh=260&mw=380&w=200&hash=A5411087D582A22AA77E2C122660E28D)