Colon Cancer Risk Factors
There are several possible risk factors for developing colon cancer or rectal cancer. Your lifestyle, diet, health conditions and family history can all play a role. While you can’t change your genetics, it may be possible to lower your risk for developing colon cancer and rectal cancer by addressing the things you can change, such as losing weight or quitting smoking.
Age
As you get older, your risk of getting colon or rectal cancer increases—with the vast majority of cases occurring in people over age 50.
The incidence of colorectal cancer in younger adults has risen steadily in recent years, but it’s still a very uncommon disease in young people. Experts have yet not identified a cause for this increase.
Lifestyle
The following lifestyle factors can increase your risk of developing colon or rectal cancer:
-
A sedentary lifestyle (physical inactivity)
-
Being overweight or obese
-
Heavy alcohol use
-
Smoking
Ethnicity
Your racial and ethnic background can also affect your risk of colorectal cancer. African Americans and Jewish people of Eastern European descent (Ashkenazi Jews) have the highest incidence of colon cancer.
Family History of Colon or Rectal Cancer (or Other Cancers)
If a member of your family—especially an immediate member like a parent, sibling or child—has had colon or rectal cancer, you are at a higher risk of developing cancer. It could be because you share a genetic predisposition or are exposed to the same environment—or both. Are there multiple instances of this disease in your family tree? Or was anyone in your family diagnosed before age 50? If so, there may be an inherited disorder in your family. Talk to your doctor about whether genetic counseling may be right for you.
In addition, if you have already been treated for one of these diseases, you are at a higher risk of developing new tumors in different areas of the colon or rectum.
Uterine cancer and ovarian cancer can be associated with colon and rectal cancers in certain genetic syndromes. If there are incidences of both colon/rectal cancer and uterine/ovarian cancer in your family, you may benefit from consulting a genetic counselor.
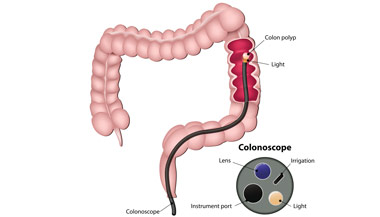
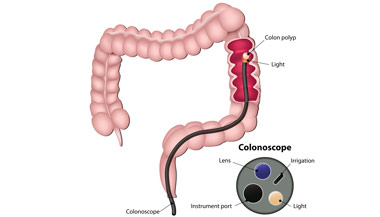
Personal or Family History of Polyps
Colorectal polyps are noncancerous growths that can occur anywhere in the colon or rectum. Although they are not cancer, polyps should be removed because they can become cancerous in the future. Individuals who have had colon or rectal polyps (especially multiple polyps) are at a higher risk for colon cancer and should be examined regularly by a doctor.
Genetic Testing for Colon Cancer at Johns Hopkins
Are you at an increased risk for colon or rectal cancer? Families with a history of colon cancer or genetic syndromes may benefit from genetic testing. Call 410-502-7082 for more information.
Inflammatory Bowel Disease
Individuals with inflammatory bowel disease (e.g., Crohn’s disease and ulcerative colitis) may experience cellular changes in the bowel due to chronic inflammation. Since these cellular changes can eventually become cancerous, patients with inflammatory bowel disease should receive screening for colon and rectal cancer early and often.
Inherited Genetic Syndromes
Approximately 5 percent to 10 percent of colon and rectal cancers are a result of an inherited genetic syndrome. These syndromes occur when a genetic mutation associated with colon or rectal cancer is passed down through a family’s genes. The two most common of these conditions are Lynch syndrome and familial adenomatous polyposis (FAP). Individuals with an inherited genetic syndrome who get colon or rectal cancer usually do so at a much younger age. Individuals with a family history of either of these genetic conditions are at a much higher risk of developing colon or rectal cancer and should be monitored by a physician.