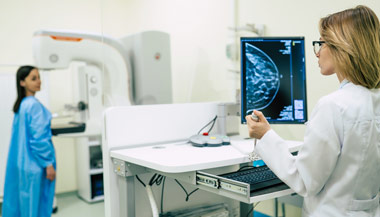
Breast Cancer: Lymphedema After Treatment
Featured Expert
Lymphedema is a problem that may occur after cancer surgery when lymph nodes are removed. Lymphedema can occur months or years after treatment. It’s a chronic (ongoing) condition that has no cure. But steps can be taken to help keep it from starting, and to reduce or relieve symptoms. If left untreated, lymphedema can get worse. Getting treatment right away can lower your risk of infections and complications.
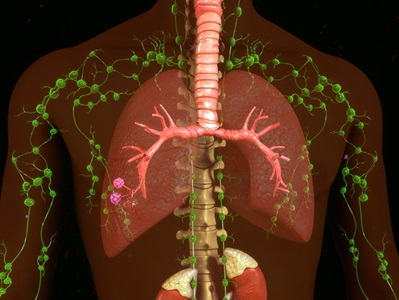
What is the lymphatic system?
The lymphatic system is a network of tiny vessels and small, bean-shaped organs called lymph nodes that carry lymph throughout the body. Lymph is a clear, colorless fluid that contains a few blood cells. It starts in many organs and tissues. The lymphatic system is part of your immune system. It helps protect and maintain the fluid balance of your body by filtering and draining lymph and waste products away from each body region. The lymphatic system also helps the body fight infection.
How Lymphedema Happens
During surgery for cancer, nearby lymph nodes are often removed. This disrupts the flow of lymph, which can lead to swelling. This is lymphedema. Lymphedema can affect one or both arm, the head and neck, the belly, the genitals, or the legs. Swelling can worsen and become severe. Skin sores or other problems can develop. Affected areas are also more likely to become infected.
Often during breast cancer treatment, some or all of the lymph nodes under the arm are treated with radiation. The lymph nodes under the arm are also called the axillary lymph nodes. They drain the lymphatic vessels from the upper arms, from most of the breast, and from the chest, neck, and underarm area.
When many lymph nodes under the arm have been removed, a woman is at higher risk of lymphedema for the rest of her life. Radiation treatments to the under arm lymph nodes can cause scarring and blockages that further increase the risk of lymphedema. Lymphedema may occur right after surgery or radiation, or months or even years later.
Types of Lymphedema
There are several types of lymphedema:
-
A mild type of lymphedema can occur within a few days after surgery and usually lasts a short time.
-
Lymphedema can also occur about 4 to 6 weeks after surgery or radiation and then go away over time.
-
The most common type of lymphedema is painless and may slowly develop 18 to 24 months or more after surgery. It does not get better without treatment.
Lymphedema can happen any time after surgery or radiation to the lymph nodes. The risk continues for the rest of the person's life. Lymphedema can’t be cured, but it can be managed. Any swelling should be checked by a healthcare provider right away.
There's no way to know who will and won't get lymphedema, but there are things that can be done to help prevent it.
Can lymphedema be prevented?
Women treated for breast cancer who have good skin care and who exercise after treatment are less likely to develop lymphedema. Newer types of lymph node surgery have also helped decrease lymphedema risk. But there is no sure way to prevent lymphedema.
Symptoms of Lymphedema
The main symptom of lymphedema after breast cancer treatment is swelling of the arm on the side where lymph nodes have been removed. The amount of swelling may vary. Some people may have severe swelling (edema) with the affected arm being several inches larger than the other arm. Others will have a milder form of edema with the affected arm being slightly larger than the other arm.
Other symptoms of lymphedema may include:
-
Feeling of fullness, heaviness, or tightness in the arm, chest, or armpit area
-
Bra, clothing, or jewelry don't fit as normal
-
Aching or new pain in the arm
-
Trouble bending or moving a joint, such as the fingers, wrist, elbow, or shoulder
-
Swelling in the hand
-
Thickening of or changes in the skin
-
Weakness in the arm
If you notice any of these symptoms, see your healthcare provider right away. Treatment needs to be started right away to keep lymphedema from getting worse.
How is lymphedema diagnosed?
There are no tests for lymphedema. Instead, your healthcare provider will ask about your medical history and give you a physical exam. You’ll be asked about:
-
Past surgeries you’ve had
-
Any problems after your surgeries
-
When the swelling started
-
If you’ve had severe swelling (edema) in the past
-
What medicines you’re taking
-
What other health conditions you have, such as high blood pressure, heart disease, or diabetes
Imaging tests, measures of volume, blood tests, and other tests may be used to diagnose lymphedema.
Treatment for Lymphedema
Treatment depends on how severe the problem is. Treatment includes ways to help prevent and manage the condition, and may include:
-
Exercise. Exercise helps improve lymph drainage. Specific exercises will be advised by your doctor or physical therapist.
-
Bandages. Wearing a compression sleeve or elastic bandage may help to move fluid, and prevent the buildup of fluid.
-
Diet and weight management. Eating a healthy diet and controlling body weight is an important part of treatment.
-
Keeping the arm raised. Raising the arm above the level of the heart when possible lets gravity help drain the fluid.
-
Preventing infection. It’s important to protect the skin in the affected area from drying, cracking, infection and skin breakdown. Your healthcare provider will advise you about how to care for your skin and nails to help prevent problems.
-
Massage therapy. Massage by someone trained in lymphedema treatment can help move fluid out of the swollen area.
Preventing Infection and Injury
Protecting the arm on the side of the surgery is very important after breast surgery. Poor drainage of the lymphatic system can cause that arm to be more at risk of infection and less sensitive to extreme temperature. Be aware of activities that put too much pressure on the affected arm. To protect your arm from injury and infection, make sure to do the following:
-
Ask for injections and blood draws to be done on the unaffected arm.
-
Ask for all blood pressure tests to be done on the unaffected arm.
-
Don't wear nightgowns or clothing with elastic cuffs or tight bands.
-
Carry your handbag or heavy packages with the unaffected arm.
-
Be very careful and use a clean razor when shaving underarms.
-
Prevent sunburns and other burns to the affected arm.
-
Wear gloves when gardening and when using strong household cleaners.
-
Clean the skin of the affected arm daily, gently dry well, and apply lotion.
-
Do approved exercises regularly to improve drainage.
-
Eat a healthy, low-sodium diet.
-
Avoid extreme hot or cold temperatures on the affected arm, such as hot tubs, saunas, and heating pads or ice packs.
-
Take good care of your fingernails and don’t cut or bite your cuticles.
-
Clean all cuts with soap and water, and then apply antibacterial ointment and a sterile dressing.
-
Protect your fingers from needle pricks and sharp objects. Use a thimble when sewing.
-
Avoid vigorous, repetitive movements against resistance, such as scrubbing, pulling, or pushing with the affected arm.
-
Tell your doctor right away if you have any signs of infection, such as redness, pain, heat, increased swelling, or fever.
Working with Your Healthcare Provider
Talk with your doctor about what you can do to try to prevent lymphedema from happening to you. Make these precautions part of your daily habits and plan to follow them for the rest of your life.
Compare your hands and arms. Look at them in the mirror. Learn what's normal for you so you can notice changes right away. If lymphedema does develop, let your doctor know right away. There are things you can do to try to keep it from getting worse.
Improving Surgical Management of Lymphedema
For patients with lymphedema, the most common treatment approach is to reduce swelling with compression and massage therapy and/or diet modification. But some patients find greater relief with surgical management. Learn more about the outpatient operation that can reroute the venous system.
LiveWell After Breast Cancer | Yoga Workout #1
LiveWell after breast cancer is The Johns Hopkins Sidney Kimmel Cancer Center initiative to get breast cancer survivors and their families moving, through fun and easy exercise routines. Exercise for every level and ability with modifications shown along the way. See more exercises for women diagnosed with breast cancer.