BPD/DS Weight-Loss Surgery
If you are extremely obese and have tried without success to get your weight under control, your healthcare provider may recommend a bariatric surgical procedure known as biliopancreatic diversion with duodenal switch (BPD/DS). This is usually known as the duodenal switch. It can help you lose more weight than either the gastric bypass or the sleeve gastrectomy. The surgery has been shown to help reduce obesity and related illnesses. These include heart disease, high blood pressure, and especially type 2 diabetes.
BPD/DS is a complex weight-loss surgery that reduces your ability to absorb calories, vitamins, and minerals. You can lose more weight with the duodenal switch than with the gastric bypass or the sleeve gastrectomy. You'll be at higher risk of developing nutritional deficiencies afterward. These include some that can be life-threatening if untreated. When deciding whether to have the surgery, these complications and other surgical risks should be carefully considered along with the benefits.
BPD/DS weight-loss surgery
Healthcare providers may recommend the BPD/DS to people who are severely obese. These people usually have a body mass index (BMI) of 50 or greater or a BMI of 40 or greater with serious type 2 diabetes and other serious health problems. These health problems include:
-
Type 2 diabetes
-
Sleep apnea
-
Heart disease
-
Lung disease
-
High blood pressure
-
High cholesterol
-
Nonalcoholic fatty liver disease
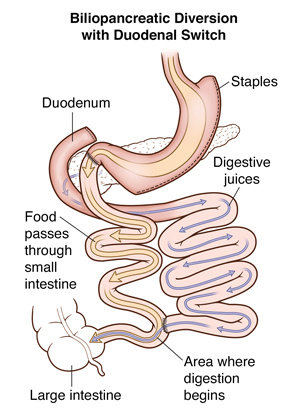
BPD/DS is a complex procedure that tackles weight loss in 3 different ways. First, a sleeve gastrectomy is performed. For this, a large portion of the stomach is removed with a stapling instrument, leaving you a narrow tube, or sleeve, from the top to near the bottom of the stomach. With less stomach to fill, you will feel full more quickly and eat less food and fewer calories.
The second part of the procedure reroutes food away from the upper part of the small intestine, which is the natural path of digestion. This cuts back on how many calories and nutrients your body is able to absorb. The small intestine is divided and a connection is made near the end of the small intestine.
The third part of the BPD/DS procedure changes the normal way that bile and digestive juices break down food. This cuts back on how many calories you absorb, causing still more weight loss. One end of the small intestine is connected to the duodenum, near the bottom of the stomach.
Open vs. laparoscopic BPD/DS
BPD/DS is done as either laparoscopic or traditional open surgery. In open surgery, the healthcare provider makes a cut in your belly area. Laparoscopic BPD/DS requires much smaller cuts and it uses small instruments with a lighted camera to perform the surgery. Laparoscopic surgery can help you recover more quickly and may reduce the risk for complications, such as infections and hernias. Some bariatric surgeons use a laparoscopic surgical robot to help do part of the operation.
Benefits of the procedure
The BPD/DS can produce a large weight loss, more than 150 pounds, because it restricts how much food you can eat and also reduces how many calories you can absorb. It helps to maintain this weight loss over many years, probably better than either the gastric bypass or the sleeve gastrectomy. It reduces the amount of fat that your body will absorb. It also helps you lose weight. If you do eat fatty meals, you may have stomach cramping and loose stools. It also helps to control diabetes over the long term, even better than the gastric bypass or the sleeve gastrectomy.
Risks of the procedure
BPD/DS reduces the absorption of essential vitamins and minerals and can result in serious, long-term complications. People who have BPD/DS may develop anemia, osteoporosis, or kidney stones.
In addition, people who have undergone BPD/DS are at high risk for calcium and iron deficiencies. These people are also at high risk for deficiencies in vitamins A, D, E, and K, the fat-soluble vitamins.
Although rare, a thiamine deficiency can happen after BPD/DS surgery. This can damage the nervous system if untreated.
Up to 18% of people with a BPD/DS surgery also develop some element of protein-energy malnutrition. When severe, this condition is known as kwashiorkor, a severe and potentially life-threatening form of malnutrition.
If you have BPD/DS surgery, you will need to take vitamin and mineral supplements and have regular blood testing for the rest of your life. This is done to prevent severe vitamin deficiencies and related complications. Even if you take the supplements as prescribed, you still may develop nutritional problems and need treatment.
Like any surgery, the BPD/DS procedure carries certain risks:
-
Internal bleeding
-
Infection
-
Blood clots in your legs that can move to the lungs
-
Hernias
-
Death
After the procedure
The American Society for Metabolic and Bariatric Surgery (ASMBS) recommends that healthcare providers prescribe these daily supplements after BPD/DS weight-loss surgery to help prevent nutritional deficiencies:
-
Vitamin A, starting 2 to 4 weeks after surgery
-
Vitamin D, starting 2 to 4 weeks after surgery
-
Vitamin K, starting 2 to 4 weeks after surgery
-
Multivitamin with 200% of the daily values, starting the first day after discharge from the hospital
-
Minimum of 18 mg to 27 mg of iron, and up to 50 mg to 100 mg a day for menstruating women or adolescents at risk for anemia
-
Calcium supplements, usually taken as 3 to 4 doses of 500 mg to 600 mg doses, starting on the first day after your discharge or within the first month after surgery. Note: Don't take these at the same time as iron supplements. Wait a couple of hours.
-
Vitamin B12 supplements containing 350 mcg to 500 mcg. Some people will need to give themselves B12 injections every month
-
Optional B-complex vitamin
-
Up to 3 servings of calcium-rich dairy beverages
The ASMBS also recommends that you eat small but nutritious meals that are high in protein, along with fruits, vegetables, whole grains, and omega-3 fatty acids. You should avoid meals high in sugar.
It's important to understand that following a healthy lifestyle is critical to maintaining weight loss after surgery. This includes eating a healthy diet and getting plenty of regular exercise. And it requires a lifelong commitment, with regular visits to your bariatric surgeon or other healthcare provider for periodic lab checks. The duodenal switch can result in considerable weight loss. It also offers improvement or resolution of many obesity-related medical conditions. But it needs regular follow-up and a commitment to taking the protein, vitamins, and supplements that you will need.





