Tibia and Fibula Fractures in Children
A bone fracture is the breaking of a bone in at least one place. The tibia and fibula are the two long bones located in the lower leg. The tibia is a larger bone on the inside, and the fibula is a smaller bone on the outside.
The tibia is much thicker than the fibula and is the main weight-bearing bone of the two. The fibula supports the tibia and helps stabilize the ankle and lower leg muscles.
What You Need to Know
- Tibia fractures are the most common lower extremity fractures in children. They account for 10 to 15 percent of all pediatric fractures.
- Fractures can be described as low-energy — caused by twisting or falls from standing height. Or high-energy — caused by high levels of force, such as a car accident or a major fall.
- A physical examination and X-rays are used to diagnose tibia and fibula fractures.
- Treatment for tibia and fibula fractures ranges from casting to surgery, depending on the type and severity of the injury.
What are tibia and fibula fractures?
Tibia and fibula fractures are characterized as either low-energy or high-energy. Low-energy, nondisplaced (aligned) fractures, sometimes called toddler’s fractures, occur from minor falls and twisting injuries. High-energy fractures, such as those caused by serious car accidents or falls, are more common in older children.
Tibia and Fibula Fractures Diagnosis
Fractures of the tibia and fibula are typically diagnosed through physical examination and X-rays of the lower extremities.
Common Types of Tibia and Fibula Fractures
There are several ways to classify tibia and fibula fractures. Below are some of the most common tibia and fibula fractures that occur in children. Sometimes they may also involve the fracture of the growth plate (physis) located at each end of the tibia.
Proximal Tibial Fractures
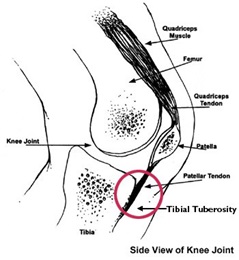
These fractures occur in the knee end of the tibia and are also called tibial plateau fractures. Depending on the location, a proximal tibial fracture may affect the stability of the knee as well as the growth plate. Common proximal tibial fractures include:
- Proximal Tibial Epiphyseal Fracture: This type of fracture affects the top portion of the bone (epiphysis) and the growth plate. Separation of the growth plate from the bone is usually caused by direct force to the knee. It’s important to have this type of fracture corrected properly, otherwise it may affect future growth and cause deformities. Treatment usually consists of setting the bone without surgery, which in some cases may be accompanied by surgical insertion of special pins or screws to secure the tibia while it heals.
- Proximal Tibial Metaphyseal Fracture (Cozen’s Fracture): This fracture affects the “neck” of the bone (metaphysis), where the tibia starts to narrow down. It is most common in children between the ages of 2 and 8. This injury can happen when force is applied to the side of the knee while the leg is extended. It is typically treated by setting the bone without surgery and using a cast to reduce movement. The cast is usually worn for about six weeks. Valgus deformity (knock knee) is one of the main potential complications after this fracture.
Tibial Shaft Fractures
This type of fracture takes place in the middle, or shaft (diaphysis), of the tibia. There are three types of tibial shaft fractures:
- Nondisplaced: A fracture where the broken bones remain aligned. This type of fracture is usually seen in children under 4. It can be caused by a mildly traumatic event or a twisting injury. Often, the first symptom is a limp. Examination usually reveals tenderness or swelling at the lower part of the tibia. The treatment typically involves immobilization in a short- or long-leg cast. The duration is three to four weeks for toddlers and six to 10 weeks for older children.
- Displaced, noncomminuted: A fracture where the bones are broken in no more than two pieces (noncomminuted) but are not aligned. This is an isolated fracture of the tibia with an intact fibula. It’s the most common tibial shaft fracture, caused by a rotational or twisting force such as a sports injury or a fall. Treatment includes setting the bone without surgery and a long-leg cast with the knee bent. Unstable displaced fractures may require surgery.
- Displaced, comminuted: A fracture where the bones are broken into several fragments and are not aligned. This fracture can be caused by high-energy trauma, such as a car accident or being struck by a vehicle. The treatment includes setting the bone without surgery and a long-leg cast worn for four to eight weeks. A short-leg weight-bearing cast may also be needed in some patients. Unstable fractures may need surgery to maintain alignment.
Distal Tibial Fractures
These fractures, also called tibial plafond fractures, take place at the ankle end of the tibia. One of the common types in children is the distal tibial metaphyseal fracture. This occurs in the metaphysis, the part of the tibia before it reaches its widest point.
These fractures are usually transverse (across) or oblique (slanted) breaks in the bone. Distal tibial metaphyseal fractures usually heal well after setting them without surgery and applying a cast. However, there is a risk of full or partial early closure of the growth plate. This may lead to a growth arrest in the form of leg length discrepancy or other deformity.
Treatment Options for Tibia and Fibula Fractures
Tibia and fibula fractures can be treated with standard bone fracture treatment procedures. The treatment approach depends on the severity of the injury and the age of the child. It may include some of the following approaches, used either alone or in combination:
- Closed reduction and immobilization: Setting the bone in place without surgery, and immobilization in a long-leg or a short-leg cast
- Open reduction: Exposing the bone surgically to set it back in place — typically performed on open fractures where the bone has punctured the skin. This procedure is usually accompanied by internal or external fixation.
- Internal fixation: Connecting the broken bones with screws, plates, rods and nails that will remain under the skin.
- External fixation: Using pins, clamps and rods to stabilize the fracture from the outside.
- Percutaneous pinning: Inserting wires across the fracture to hold the pieces in place until they heal. The wires are removed after the fracture has healed.
- Medications: When the fracture has broken the skin, treatment may include antibiotics to prevent infection and analgesics to control pain. A tetanus shot may also be needed.
Treatment of Open Fractures of the Tibia
An open fracture occurs when the bone or parts of the bone break through the skin. This type of fracture usually results from high-energy trauma or penetrating wounds. Open fractures of the tibia are common among children and adults.
The treatment of an open tibial fracture starts with antibiotics and a tetanus shot to address the risk of infection. Then the injury is cleaned to remove any debris and bone fragments. Surgery may also be needed depending on the wound size, amount of tissue damage and any vascular (circulation) problems. Open reduction and internal fixation is the surgery that can be used to reposition and physically connect the bones in an open fracture.
Wounds may be treated with vacuum-assisted closure. This procedure involves placing a piece of foam in the wound and using a device to apply negative pressure to draw the edges of a wound together.
Alternate methods can include repeated cleanings before closing the wound, or an external fixator to repair the wound surgically.
Rehabilitation After Tibia and Fibula Fractures
People with bone fractures in the leg may need an assistive device, such as crutches, to keep the weight off the leg while the fracture heals.
A physical therapist will provide instructions on how to use crutches or another assistive device, including how to walk up and down stairs or to get in and out of a car. The doctor may provide weight-bearing restrictions to follow. A physical therapist can help the child maintain these restrictions to ensure the child does not put too much stress on the healing bone.
After the cast is removed, working with a physical therapist often helps restore function in the leg. The immobilized body part is generally stiff and difficult to move after being freed. The longer the immobilization, the stiffer it can become, because muscles and other connective tissues have weakened due to lack of use, and can also shrink, limiting normal motion.
Early physical therapy is important to encourage full recovery and prevent re-injury and chronic issues related to immobilization by the cast. With daily use of the affected limb, the range of motion is usually regained. However, a physical therapist can help the child recover more safely and quickly by engaging in exercise, stretching and other therapeutic activities. Physical therapy also helps retrain balance, improve walking and allow for safe return to daily activities.
For young athletes and other active people, physical therapy may include higher-intensity exercises such as plyometric (vigorous drills), proprioceptive (stimulating the muscles and tendons) and sport-specific training. This rehabilitation plan helps ensure a safe return to the desired activity level.