Patient Story
Prematurity: Mia’s Story
Patient Story Highlights
- Mia was born weighing only 350 grams — 0.77 pounds.
- When she was only seconds old, Oscar Winners, M.D. intubated his tiniest patient. It’s a medical procedure where a flexible plastic tube is inserted into the trachea to help babies breathe with a machine.
- Mia grew stronger for the next 172 days she spent in the NICU.
- It takes a village to take care for any NICU baby. We care for the baby as a whole — the brain, the heart, all the vital organs, but with prematurity a primary limiting factor is always the lungs.

When their daughter was born weighing only 350 grams — 0.77 pounds — Jessica and Matthew recognized her chances of survival were as small as she was. “We knew it was against all odds. Our friends and her grandparents were calling all of their friends at church to pray for Mia. We had like a thousand people praying,” Jessica says.
Included was Oscar Winners, M.D., a neonatologist at Johns Hopkins All Children’s Hospital, who also asked his own daughter to remember a special patient in her prayers. Mia is the smallest patient he has ever helped care for — a rare distinction for a Level IV neonatal intensive care unit (NICU) where the most complex and critical newborn infants are taken.
Jessica was hospitalized for a week before delivery as every effort was exhausted to prolong her pregnancy so her baby could develop and grow stronger. Although doctors hoped for more than 24 weeks gestation, Mia’s arrival was not a surprise to an army of clinicians at the ready in the NICU at Johns Hopkins All Children's in St. Petersburg, Florida. When she was only seconds old, Winners intubated his tiniest patient. It’s a medical procedure where a flexible plastic tube is inserted into the trachea to help babies breathe with a machine. Tiny Mia’s determination to live despite her size quickly won a special place in his heart.
With breathing assisted by a ventilator, her care team’s next challenge was an umbilical artery catheter, or UAC, which allows blood pressure monitoring and testing without repeated needle sticks. “On a baby of Mia’s size, it’s like trying to thread a hair inside a piece of thin spaghetti,” says Tifani Russell, APRN, who’s an ace at the task under tremendous pressure.
Before driving to work when Mia was 3 days old, Winners checked the infant’s oxygen levels from his home. “Her labs are good. Finally, it’s going to be a good day,” he recalls. He had been trying since her birth to open a collapsed lung and was delighted to see better oxygen levels. “It was my daily problem to open that lung. Today might be the day,” he says.
But Mia again tested her care team’s skills, and the faith of a thousand prayers. By 8:15 a.m., she suffered a pulmonary hemorrhage, her frail, underdeveloped body began bleeding internally. Her oxygen levels were plummeting. Things were not looking good. The doctor’s glee was gone as he dialed Jessica’s cell phone to tell her return to the hospital immediately. This was the phone call they both feared. “I told him I was only two blocks away,” Jessica recalls. “I turned the corner and tossed the keys to the valet and ran to the elevator. I started to panic running to the NICU.”

Mia was struggling. Winners was worried his tiniest patient was giving up. Matthew raced to join his wife. Doctors, nurses, respiratory therapists and other staff members convinced the couple that it was time to hold Mia. “They were preparing us if we had to say goodbye,” remembers Jessica.
With Mia in her arms for the very first time, Jessica recalls the faces of the medical team surrounding her. “You could tell they were prepared for her not to make it. But you could also tell THEY believed that WE believed she would. I can’t thank them enough for that,” emotion coloring her voice.
Mia had been detached from the mechanical ventilator, so Alexis Benz, R.N., and Tricia Mason, R.T., manually bagged her through her intubation tube so Jessica and Matthew could each hold their daughter close. The situation was dire. Dry eyes were scarce in the room of hard-core baby savers.
But somewhere between mom’s soothing snuggles and dad’s delicate hugs, Mia’s heart rate started to improve. “She threw out the medical books,” Jessica says. Her oxygen levels slowly improved. The care team was encouraged, but Winners still worried about possible brain damage from the pulmonary hemorrhage on a neonate of such minuscule weight. Complications are common for preemies with undeveloped lungs and immature immune systems. Mia would have to leave mom’s arms for X-rays and an ultrasound of her head. The images would tell the team if there was any permanent damage from her hemorrhage.
“It was one of the best X-rays I’ve even seen,” Winners recalls. “That lung I had been trying to open for three days was open.” But it isn’t until radiologist Javier Quintana, M.D., called with the words, “The head is fine. There’s no bleed,” that Winners became jubilant and rushed back to the bedside. Mia was back. Matthew tapped his heart twice and pointed to heaven. His tiny daughter just earned a new moniker — Miracle Mia.
“God took her,” chokes out Winners. “That’s why she’s going to be in my head and in my heart for life.”
“She’s his angel baby,” Jessica says.
Mia grew stronger for the next 172 days she spent in the NICU. And an intestinal perforation weeks later required two surgeries to repair. “Every single complication that she had during her entire admission was like, ehhh, that’s OK, I’m fine,” Winners jests as if speaking for Mia.
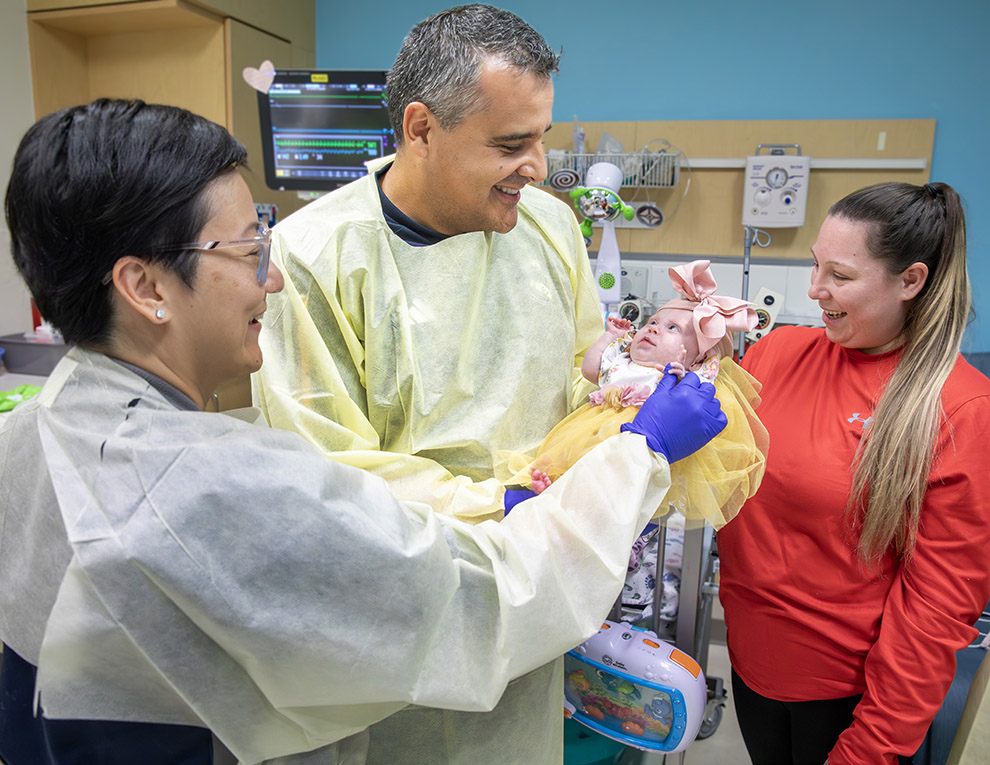
“Because of that day, a lot of doctors would stop by her room just to see her, just to reel themselves back in after something stressful,” Jessica says. “They love to just hold her.”
They are recharged by a smile beneath one of more than 100 bows that adorn her daughter’s head. Mia’s hair hasn’t grown in yet and Jessica wants to be sure everyone knows this little fighter is all girl. “They helped grow this baby out of utero almost exactly as she would have grown inside. They grew her outside of a mother’s belly, it’s just amazing.”
“It takes a village to take care for any NICU baby,” says neonatologist Lilly Chang, M.D. It starts with the affectionately-named Stork Team of Johns Hopkins All Children’s Hospital physicians, nurses and respiratory therapists who are present in the delivery room and transport newborns to the NICU. “We care for the baby as a whole — the brain, the heart, all the vital organs, but with prematurity a primary limiting factor is always the lungs. Are we able to get oxygen to the brain?”she says. “We have a large staff on hand and Jessica was very, very involved, which is supremely important to family-centered care. She was an expert on Mia, which is the way it should be. She knew this was going to be a long, hard road, a roller coaster.”
“Mia is more than just a miracle, she’s a testament to the invaluable role a dedicated and involved family plays in the success of our patients,” adds Noura Nickel, M.D., one of Mia’s neonatologists during her 175 days in the NICU. “Mia’s mom was actively at her bedside through all the ups and downs, engaged with the team members and she’s the reason Mia thrived in the NICU and will continue to thrive in the long run. Parent and care partner involvement is so important to the success of these babies in the short and long term.”
“There’s nothing wrong with her, except that she’s little, but she can’t help that,” Jessica says. “When we’re out in public people ask if she’s real. They think she’s one of those Baby Alive dolls.”
She proudly replies, “Oh, she’s real. She’s very real.”
Mia's Care Team
-
Oscar Gaston Winners Mendizabal, MD

Expertise: Neonatology
Primary Location: Johns Hopkins All Children's Hospital, Saint Petersburg, FL
-
Javier Francisco Quintana, MD

Expertise: Pediatric Radiology
Primary Location: Johns Hopkins All Children's Hospital, Saint Petersburg, FL
-
Lilly Lan Chang, MD

Expertise: Neonatology
Primary Location: Johns Hopkins All Children's Hospital, Saint Petersburg, FL
-
Noura Estephane Nickel, MD

Expertise: Neonatology
Primary Location: Johns Hopkins All Children's Hospital, Saint Petersburg, FL





