Rheumatic Heart Disease
What is rheumatic heart disease?
Rheumatic heart disease is a condition where the heart valves have been permanently damaged by rheumatic fever. The heart valve damage may start shortly after untreated or undertreated streptococcal infection, such as strep throat or scarlet fever. An immune response causes an inflammatory condition in the body. This can result in ongoing valve damage.

What causes rheumatic heart disease?
Rheumatic heart disease is caused by rheumatic fever. This is an inflammatory disease that can affect many connective tissues, especially in the heart, joints, skin, or brain. The heart valves can be inflamed and become scarred over time. This can result in narrowing or leaking of the heart valve. This makes it harder for the heart to work normally. This may take years to develop and can lead to heart failure. Rheumatic fever can occur at any age. But it often occurs in children ages 5 to 15. It’s rare in developed countries like the U.S.
Who is at risk for rheumatic heart disease?
Untreated or undertreated strep infections can increase the risk for rheumatic heart disease. Children who get repeated strep throat infections are at the most risk for rheumatic fever and rheumatic heart disease.
What are the symptoms of rheumatic heart disease?
A recent history of strep infection or rheumatic fever is key to the diagnosis of rheumatic heart disease. Symptoms of rheumatic fever vary. They typically start 1 to 6 weeks after a bout of strep throat. In some cases, the infection may have been too mild to be recognized. Or it may be gone by the time the person sees a healthcare provider.
These are the most common symptoms of rheumatic fever:
-
Fever
-
Swollen, tender, red, and very painful joints (very often the knees and ankles)
-
Lumps under the skin (nodules)
-
Red, raised, lattice-like rash, often on the chest, back, and belly
-
Shortness of breath and chest discomfort
-
Uncontrolled movements of arms, legs, or facial muscles
-
Weakness
Symptoms of rheumatic heart disease depend on the degree of valve damage and may include:
-
Shortness of breath (very often with activity or when lying down)
-
Chest pain
-
Swelling
How is rheumatic heart disease diagnosed?
People with rheumatic heart disease will have or recently had a strep infection. A throat culture or blood test may be used to check for strep.
They may have a murmur or rub that may be heard during a routine physical exam. The murmur is caused by blood leaking around the damaged valve. The rub is caused when the inflamed heart tissues move or rub against each other.
Along with a complete health history and physical exam, tests used to diagnose rheumatic heart disease may include:
-
Echocardiogram (echo). This test uses sound waves to check the heart's chambers and valves. The echo sound waves create a picture on a screen as a handheld ultrasound probe (transducer) is passed over the skin over the heart. Echo can show damage to the valve flaps, backflow of blood through a leaky valve, fluid around the heart, and heart enlargement. It’s the most useful test for diagnosing heart valve problems. For more in-depth pictures, you may be given sedation, and the probe is put into the throat (transesophageal echo or TEE).
-
Electrocardiogram (ECG). This test records the strength and timing of the heart's electrical activity. It shows abnormal rhythms (arrhythmias or dysrhythmias). And it can sometimes find heart muscle damage. Small sensors are taped to your skin to pick up the electrical activity.
-
Chest X-ray. An X-ray may be done to check your lungs and see if your heart is enlarged.
-
Cardiac MRI. This is an imaging test that takes detailed pictures of the heart. It may be used to get a more exact look at the heart valves and heart muscle.
-
Blood tests. Certain blood tests may be used to look for infection and inflammation.
How is rheumatic heart disease treated?
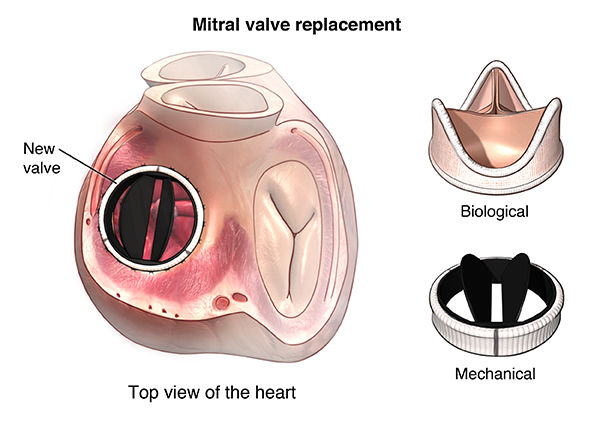
Treatment depends in large part on how much damage has been done to the heart valves. In severe cases, treatment may include surgery to replace or fix a badly damaged valve.
The best treatment is to prevent rheumatic fever. Antibiotics can often treat strep infections and keep rheumatic fever from occurring. Anti-inflammatory medicines may be used to reduce inflammation and lower the risk of heart damage. Other medicines may be needed to manage heart failure.
People who have had rheumatic fever are often given daily or monthly antibiotic treatments. These can prevent infections from occurring again. They can also lower the risk of more heart damage. To reduce inflammation, aspirin, steroids, or nonsteroidal anti-inflammatory drugs (NSAIDs) may be given.
Treatment The Johns Hopkins Center for Cardiac Immunology

The Johns Hopkins Center for Cardiac Immunology delivers care to individuals with heart conditions resulting from immune system abnormalities. The center combines the expertise of clinicians and researchers in cardiology and immunology to offer superior clinical care and promote advancements in scientific knowledge.
What are possible complications of rheumatic heart disease?
Some complications of rheumatic heart disease include:
-
Heart failure. This can occur from either a severely narrowed or leaking heart valve.
-
Bacterial endocarditis. This is an infection of the inner lining of the heart. It may occur when rheumatic fever has damaged the heart valves.
-
Complications of pregnancy and delivery due to heart damage. Women with rheumatic heart disease should discuss their condition with their healthcare provider before getting pregnant.
-
Ruptured heart valve. This is a medical emergency. It must be treated with surgery to replace or fix the heart valve.
What can I do to prevent rheumatic heart disease?
Rheumatic heart disease can be prevented by preventing strep infections. Or by treating them with antibiotics when they do occur. It’s important to take antibiotics as prescribed. Always finish taking them as instructed, even if you feel better after a few days.
Living With Rheumatic Heart Disease
You will need to have ongoing follow-up with your healthcare provider to check the condition of your heart. Depending on the amount of heart damage, you may have some activity restrictions. Your provider may advise that you take antibiotics for a longer time to prevent another infection of rheumatic fever.
When should I call my health-care provider?
If your symptoms get worse or you have new symptoms, call your health-care provider.
Key Points About Rheumatic Heart Disease
-
Rheumatic heart disease is a condition where the heart valves have been permanently damaged by rheumatic fever.
-
Rheumatic fever is an inflammatory disease that can affect many connective tissues, especially in the heart.
-
Untreated or undertreated strep infections put a person at increased risk. Children who get repeated strep throat infections are at the most risk for rheumatic fever and rheumatic heart disease.
-
A recent history of strep infection or rheumatic fever is key to the diagnosis of rheumatic heart disease.
-
Treatment depends on how much damage has been done to the heart valves. It may even include surgery to replace or fix a badly damaged valve.
Checkmark Stay on Top of Your Heart Health
If you have a new or existing heart problem, it's vital to see a doctor. Our heart health checklist can help you determine when to seek care.