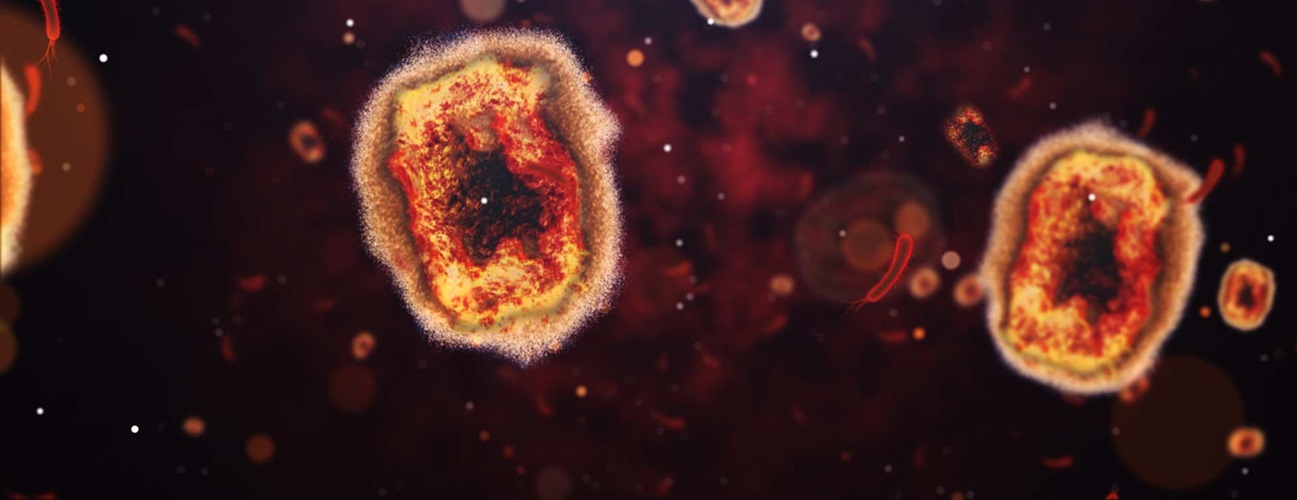
Mpox
Updated Aug. 16, 2024
Mpox, formerly called monkeypox, is an infection caused by a virus. Noreen Hynes, M.D., M.P.H., is the director of Johns Hopkins’ Geographic Medicine Center of the Division of Infectious Diseases. Amita Gupta, M.D., M.H.S., is chief of Johns Hopkins’ Division of Infectious Diseases. Together, they review what the public should know about mpox, how it’s spread and its impact on health.
What You Need to Know
- On Aug. 14, 2024, the World Health Organization declared a public health emergency for the ongoing mpox outbreak in Africa.
- The general risk to the U.S. is considered low at this time.
- Mpox is spread by exposure to, or direct contact with, an infected person.
- Mpox can cause a rash, swollen lymph nodes, fever, muscle aches and other symptoms.
- While some strains of mpox can cause severe disease, the infection most often clears up on its own.
- Vaccines can prevent mpox in some people who are at risk.
On This Page:
Overview | Symptoms | Causes | Diagnosis | Types | Treatment | Prevention & Exposure
What is mpox?
Mpox is an infection caused by a virus similar to the smallpox virus. In some countries, mpox disease has been endemic ― occurring among the general population ― for many years.
Mpox was first identified in 1958 in imported captive research African monkeys and was later found in tropical rain forests in Central and West African countries. The first human case was identified in 1972 among people living at the edge of the rain forests.
Individual cases and outbreaks have occurred in these countries, and there had been rare outbreaks in other areas from time to time. Then, in 2022, the World Health Organization (WHO) declared a global health emergency due to the spread of mpox more widely around the world, with about 100,000 cases and 208 deaths. A concerted effort to address the outbreak with effective prevention and treatment resulted in a dramatic drop in cases.
Mpox Outbreak 2024
On August 14, 2024, a new mpox public health emergency was declared by the WHO because Africa is now experiencing the largest epidemic of mpox that it has ever experienced. For example, the Democratic Republic of Congo has reported about 15,600 cases and 537 deaths as of August 14,2024, with most cases occurring in children. Also, several previously mpox-free African countries are now reporting cases.
Mpox disease may be more likely to affect people or be more severe in people who have never been vaccinated against smallpox. The smallpox vaccination program ended in the U.S. in 1972. Then, in 1980 the WHO declared smallpox virus to be eradicated and routine smallpox vaccinations ended worldwide.
Are there different types of mpox?
Yes, there are two strains or subtypes of mpox, labeled clade I and clade II. The strain that is endemic in several countries in West Africa, which was seen in outbreaks outside of Africa in 2022, clade II with 2 subdivisions – IIa and IIb, is less severe than the strain that occurs in the Congo basin in Central Africa, clade I
What is the risk of mpox in the U.S.?
The risk to the general U.S. population from clade I and clade Ib now circulating in the Democratic Republic of Congo is considered to be very low and there are no known cases in the U.S. at this time.
Mpox Symptoms
Mpox has a long incubation period. That means it can take three to 21 days to develop illness after being exposed to the virus. However, a person can transmit the disease to someone else one to four days before symptoms appear. Altogether, mpox infection lasts two to four weeks.
- Mpox symptoms in humans usually start with a general, all-over feeling of being ill.
- Flu-like symptoms such as fever and muscle aches develop.
- Lymph nodes become swollen, often at the time of fever onset. This is seen in most cases and is usually seen before the rash. This feature distinguishes this infection from smallpox.
- A few days later, a rash may appear on the hands, feet, chest, face or mouth, or near or on the genitals. Mpox may initially be mistaken for chickenpox or a sexually transmitted disease if the rash is in the genital or anal region.
The rash progresses through several stages:
- A small, raised solid pimple or swelling (called a papule) appears.
- A blister-like rash (consisting of vesicles) that looks like chickenpox develops.
- The rash may begin on the face and spread elsewhere on the body, or, if acquired during intimate or sexual contact, may begin in the genital or perianal areas.
Who is at risk for severe mpox?
Mpox may be most severe in people with weakened immune systems, in young children, especially those who are malnourished, and, possibly, pregnant persons. In previous outbreaks, fatal cases have occurred, primarily among children in Africa.
What causes mpox?
Mpox is caused by a virus related to the one that causes smallpox, but mpox disease is usually milder than smallpox. The virus can be spread through direct contact with an infected person, specifically contact with their saliva, nasal mucus or areas around the anus, rectum or vagina.
Activities that can transmit from an infected person to an uninfected person include:
- Sharing space in a crowded household
- Prolonged face-to-face contact
- Hugging, massage and kissing
- Oral, anal or vaginal sex
- Touching the genitals — penis, testicles or labia (lips of female genitals) — vagina or anus of a person infected with mpox
In rare cases, a person can contract mpox by touching objects, fabrics and surfaces that were used by a person with mpox but were not disinfected. This can include bedding, clothing, towels and sex toys.
There is no evidence that people who are exposed to a person with mpox but never have symptoms can spread the illness.
Mpox Diagnosis
A health care professional can identify mpox with a sample of fluid swabbed from the rash. Your doctor may need to rule out other rash-producing illnesses such as chickenpox, measles or syphilis, as well as screen for sexually transmitted diseases such as HIV, syphilis and others.
Is mpox treatable?
Although mild cases resolve on their own, people who become very sick from mpox can be treated with antiviral agents. Smallpox therapies may be used, although data on their effectiveness for either clade I or clade II mpox infection is limited.
The Centers for Disease Control and Prevention (CDC) suggests that people at risk for severe mpox disease may benefit from antiviral treatment with a drug called tecovirimat. This antiviral is being studied in the Democratic Republic of Congo and preliminary results have just been released which show it is safe but it may not be better than placebo for resolving symptoms and skin lesions due to clade 1b infection. An additional trial is currently underway in the US to see if it is safe and effective in easing mpox symptoms that are due to clade 2 primarily.
What if I am pregnant or breastfeeding?
There is limited information on mpox’s effect on people who are pregnant or breastfeeding. Symptoms and signs in this group are similar to those seen in people with mpox who are not pregnant or breastfeeding. But, it is unknown if pregnant persons are more susceptible to infection. It is unknown if mpox virus is present in breastmilk.
Mpox can be passed to the fetus during pregnancy or to the newborn baby by contact with the mpox rash or sores during and after birth. Mpox in pregnancy can also lead to miscarriage, a baby being born too early (premature labor), or even a fetal death before delivery.
For information on what to do if you are pregnant or breastfeeding and exposed to mpox, follow the guidelines provided by the CDC. The World Health Organization also has additional resources.
How to Prevent Mpox
The best ways to keep from getting sick with mpox are:
- Avoid close contact with people who are infected or their personal belongings, bedding and other high-contact items.
- Wash your hands frequently and thoroughly.
- Wear a mask and gloves or other protection when caring for someone with mpox or disease symptoms.
- The WHO has suggested limiting the number of sexual partners.
Mpox Vaccine
There is an FDA-licensed and approved two-dose vaccine to prevent mpox. When given early enough after exposure (within four days), vaccines may lessen the severity of the disease. Health care professionals may recommend vaccines for those who have been in close contact with a person who is infected.
Mpox vaccination can help prevent getting the disease. Data from the CDC show that the vaccine most widely used in the U.S. is 75% effective with one dose and 66% to 86% effective with two doses given 28 days apart in persons with normal immune systems. In immunocompromised persons the vaccine was about 51% effective after one dose and 70% after 2 doses given 28 days apart. Other vaccines are under investigation.
The mpox vaccine may be appropriate to protect at-risk populations, such as:
- People with weakened immune systems
- Researchers working with the mpox virus
- Men who have sex with men, transgender or nonbinary people, who in the past six months have had any of the following:
- A new diagnosis of one or more sexually transmitted diseases
- More than one sex partner
- Sex at a commercial sex venue
- Sex in association with a large public event in a geographic area where mpox transmission is occurring
- Sexual partners of persons with the risks described above
- People who anticipate experiencing any of the above
- Although there have been no clade I cases of mpox identified in the U.S., the CDC recommends that people in the U.S. who are exposed to or at high risk for catching mpox should get vaccinated.
- However, the vaccine is NOT approved for use in persons without one or more of the above risk factors who are traveling to affected African countries.
If you are pregnant or breastfeeding and exposed to mpox, consult with your doctor about the risks and benefits of getting the mpox vaccine and decide together if it is an appropriate choice for you.
What to Do If You Are Exposed to Mpox
According to the CDC, people who have been exposed to an infected person or animal should follow these steps:
- If you are pregnant or breastfeeding, mpox could harm your fetus or infant. Contact your doctor right away and follow these CDC guidelines.
- Watch for mpox signs and symptoms for three weeks after exposure.
- Talk to your doctor and see if you can be vaccinated as soon as possible after exposure to someone with mpox. Getting the vaccine within four days of exposure provides the best chance to prevent the disease or make it less severe, but getting it up to 14 days post-exposure may help protect you.
- If you develop a new rash, contact your doctor.
- Do not touch or scratch the rash, which can spread it. Cover the rash with clothes or gloves, bandages or a mask.
- Tell any care providers treating you in person that you have been exposed to mpox.
- Isolate and do not share items you have touched.
- Inform care providers, roommates, sex partners and anyone with whom you’ve shared utensils or had prolonged skin-to-skin contact that you have been exposed to mpox.
- If you become ill, follow CDC guidelines for what to do if you become sick from mpox.
Is mpox fatal?
It can be. Some strains of mpox have a death rate ranging from 1% to 10%, based on data from cases in some African countries. During the July 2022 to May 2023 global outbreak, the strain circulating is associated with a 1% or lower death rate. The current African clade I epidemic has a death rate of about 4%.
Will there be an mpox pandemic?
An mpox pandemic is unlikely for several reasons:
- The mpox virus is not new. What has changed over the last few years is the patterns of infection among people as well and genetic characteristics of the clade I virus
- Vaccines that can help lessen the impact of this disease are already available. WHO is deploying vaccines to affected African countries to help control spread of the virus.
- Since mpox transmission requires person-to-person contact, it is less likely than other viruses (such as SARS-CoV-2, which causes COVID-19) to spread among large numbers of people who do not have close physical contact.