Hip Arthritis
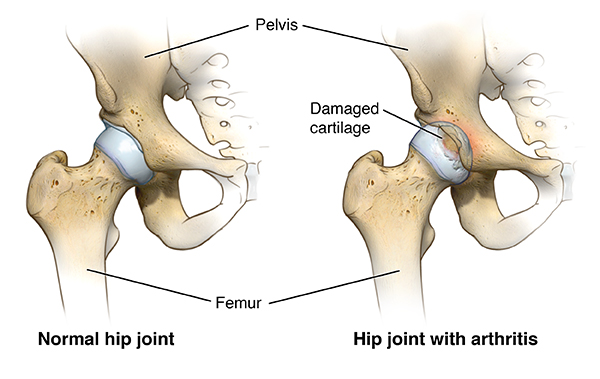
Hip arthritis is cartilage damage in the hip joint. It’s a common condition that can be painful and worsen over time, affecting your mobility and quality of life.
What You Need to Know
- There are several types of hip arthritis, including osteoarthritis, rheumatoid arthritis, psoriatic arthritis and post-traumatic arthritis.
- The causes of hip arthritis vary depending on the type. The most common cause is age-related wear and tear in the hip joint.
- Symptoms of hip arthritis may include pain in or near the hip joint, stiffness, audible clicking sounds when moving the hip, and weakness.
- While hip arthritis is usually a chronic condition, there are treatments to help ease the symptoms and reduce further damage. If your quality of life suffers, surgery such as hip replacement can provide long-term relief.
What is hip arthritis?
Hip arthritis is deterioration of the cartilage of the hip joint. The hip is a ball-and-socket joint with the ball at the top of the thighbone (the femoral head). The ball is separated from the socket (the acetabulum) by cartilage. The cartilage acts as a slippery coating between the ball and the socket that allows the ball to glide and rotate smoothly when the leg moves. The labrum, a strong cartilage that lines the outer rim of the socket, provides stability.
When cartilage in the hip is damaged, it becomes rough. Thinning of cartilage narrows the space between the bones. In advanced cases, bone rubs on bone, and any movement can cause pain and stiffness. When there is friction at any point between bones, it can also lead to bone spurs — bone growths on the edges of a bone that change its shape.
Types and Causes of Hip Arthritis
Osteoarthritis of the Hip
Osteoarthritis is a degenerative joint disease, which means it causes gradual damage to the joint. It is the most common form of hip arthritis and can affect other joints. Hip osteoarthritis is typically caused by wear and tear related to aging and worsens over time. The breakdown of cartilage leads to pain and inflammation.
Hip osteoarthritis may develop faster in some people due to irregular shape of the bones forming the hip joint. For example, if the ball and the socket parts of the hip joint don’t perfectly fit together (a condition resulting in hip impingement), they may rub against each other, eventually leading to osteoarthritis. This may also happen in people with hip dysplasia, who have a hip socket that is too shallow to support the ball of the femur. This places abnormal stress on the cartilage, causing it to wear away prematurely.
Stages of Osteoarthritis of the Hip
- Stage 1: Minor wear and tear of the hip joints and minor bone spurs, often with little to no pain.
- Stage 2: The cartilage begins to break down, and bone spur growths are often visible on X-rays. Symptoms include pain, discomfort and stiffness in the hip. This stage is also called mild hip osteoarthritis.
- Stage 3: The cartilage starts to erode and the gap between the hip bones narrows. Normal activities such as walking, kneeling or squatting cause pain and swelling. This stage is also called moderate hip osteoarthritis.
- Stage 4 (the most severe stage): The cartilage is almost gone, which causes chronic inflammation. Pain and stiffness are felt almost all of the time.
Rheumatoid Arthritis of the Hip
Rheumatoid arthritis (RA) is a disease resulting from the immune system attacking healthy tissue in the joints, including the hip. It causes inflammation of the synovial membrane, the capsule surrounding the hip joint. Inflammatory cells release substances that break down hip cartilage over time. RA typically affects smaller joints such as the wrist and fingers first, and may not be noticeable in the hip until it causes symptoms.
Psoriatic Arthritis of the Hip
Psoriatic arthritis is a type of arthritis that can develop in people with psoriasis, an autoimmune skin condition that can also cause inflammation in the joints, including the hip. Over time, untreated inflammation can lead to joint damage. Psoriatic arthritis of the hip is a chronic condition. It can develop before or after the telltale skin symptoms of psoriasis develop.
Post-Traumatic Hip Arthritis
Injury or trauma to the hip, such as hip fracture, may lead to development of arthritis later in life. Trauma such as falls, sports injuries and car accidents can damage the cartilage. While the injury itself may heal, the cartilage damage and any changes in the hip joint alignment or anatomy can lead to arthritis years later.
Hip Arthritis Due to Avascular Necrosis
Avascular necrosis happens when a bone loses its blood supply and starts to collapse. In the hip, avascular necrosis may develop in the femoral head (the ball part of the hip joint). As the bone tissue dies, the femoral collapses and loses its shape, which eventually leads to severe hip arthritis.
Hip Arthritis Symptoms
Symptoms of hip arthritis can be constant or flare up. Common hip arthritis symptoms include:
- Pain in or near the hip that can worsen due to certain movements and exercises. Cartilage wears down unevenly, and if a particular movement places stress on an area with more damage, pain increases. With hip arthritis, the pain is mainly felt in the groin, and occasionally in the outer thigh and upper buttock area. Pain can get worse after standing or walking for long periods of time or after a period of rest (waking up in the morning).
- Stiffness in the hip makes it difficult to move the hip or rotate the leg. This may make daily activities, such as putting on socks and shoes, difficult.
- Crepitus is the audible cracking, crunching, clicking or snapping sound you hear when moving a damaged hip.
- Weakness in the hip is often a result of reduced activity. Hip arthritis may cause you to move less due to pain, which makes the joint even weaker and worsens symptoms.
Risk Factors for Hip Arthritis
- Age. The older you are, the more likely you have worn out the cartilage in your hip joint.
- Excess weight. Being overweight or obese puts additional stress on the hips.
- Injury. Severe injury, such as a hip fracture or labral tears, can cause arthritis years later.
- Overuse. Jobs and sports that require physically repetitive motions that place stress on the hip can increase risk for developing osteoarthritis.
- Gender. Women who are postmenopausal are more likely to develop hip osteoarthritis than men. Rheumatoid arthritis affects women more than men.
- Structural or developmental abnormalities. Irregularly shaped bones forming the hip joint, such as with hip dysplasia and impingement, can lead to abnormal stress on the cartilage.
- Autoimmune triggers. While the causes of rheumatoid arthritis and psoriatic arthritis remain unknown, triggers of autoimmune diseases are an area of active investigation. For example, infection is believed to be one of the triggers for psoriasis.
- Genetics. Certain autoimmune conditions that lead to hip arthritis may run in the family.
- Other health conditions. People with diabetes, high cholesterol, hemochromatosis (high levels of iron in the blood) and vitamin D deficiency are more likely to develop osteoarthritis.
How is hip arthritis diagnosed?
Your doctor may use the following diagnostic tools to determine if you have hip arthritis:
- Medical history and physical examination
- Blood tests for genetic markers and/or RA antibodies
- X-rays to determine cartilage loss
You can’t see cartilage on X-ray, but you can see the space between the bones of the hip joint. If it’s narrowing, this could mean that cartilage has been lost. X-rays also show bone spurs and cysts, which develop due to osteoarthritis. MRI of the hip is usually not needed to diagnose arthritis.
Hip Arthritis Treatment
Treatment options for hip arthritis vary depending on the type and stage of the disease, your age, severity of pain and other factors. While doctors can’t reverse cartilage loss, there are ways to improve pain and prevent further damage.
Nonsurgical Treatments for Hip Arthritis
- Activity modifications may help reduce painful flare-ups. Avoid activities that aggravate hip arthritis, such as running, jumping and other high-impact exercises.
- Lifestyle modifications, such as weight loss, can help reduce stress on the hip joint.
- Physical therapy exercises can help improve strength in the hip. Engaging in low-impact exercises and activities, such as swimming and cycling, and remaining physically active are key to managing hip arthritis symptoms.
- Heating pads can help soothe inflammation in the hip.
- Medications and injections, such as corticosteroid injections, hyaluronic acid injections, platelet-rich plasma injections, vitamin and mineral supplements, and immunosuppressive or biologic medicines can help control pain and inflammation. Which medications will work best depends on the type of arthritis.
- Walking aids such as a cane or walker provide support when walking.
Surgery for Hip Arthritis
The progression of hip arthritis and effectiveness of various nonsurgical treatments varies. If nonsurgical options don’t provide the desired pain relief and your quality of life suffers, it may be time to consider surgical options, such as:
- Hip replacement surgery, or hip arthroplasty, is a procedure to replace one or both ends of a damaged hip joint with artificial implants.
- Hip fusion is a procedure to fuse the bones of the hip joint together. It used to be the standard surgical treatment for hip arthritis before replacement surgeries became available, but is now a last-resort treatment as it severely impacts mobility.





.png?h=170&iar=0&mh=260&mw=380&w=200&hash=A5411087D582A22AA77E2C122660E28D)
