Hiatal Hernia
What is a hiatal hernia?
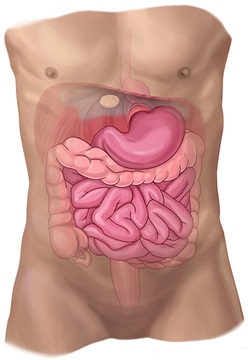
Unlike ventral hernias, which protrude through the abdominal wall, a hiatal hernia occurs when the upper part of the stomach pushes up into the chest through a small opening in the diaphragm, the muscle that separates the abdomen from the chest. A hiatal hernia results in retention of acid and other contents since the stomach tends to get squeezed by this opening in the diaphragm. These acids and other substances can easily back up — reflux or regurgitate — into the esophagus.
There are four types of hiatal hernias. The vast majority of hiatal hernias are called type I, or sliding hiatal hernias. In this type, the stomach intermittently slides up into the chest through a small opening in the diaphragm. Type II, III and IV hiatal hernias are called paraesophageal hernias. They occur when a portion of the stomach pushes up into the chest adjacent to the esophagus.
Hiatal Hernia Causes
Hiatal hernias can occur for a number of reasons, including:
-
Being born with an unusually large hiatus
-
Injury or trauma to the area such as force from a seatbelt during an accident
-
Obesity
-
Persistent and intense pressure on the surrounding muscles caused by:
-
Chronic coughing
-
Lifting heavy objects
-
Repetitive vomiting
-
Straining during a bowel movement
-
Hiatal Hernia Diagnosis
To identify a hiatal hernia, a health care provider may use multiple diagnostic techniques but will begin with a medical history and physical examination. The provider will inquire about and/or look for:
-
Acid reflux
-
Acidic or “sour” taste in the back of the mouth or throat
-
Anemia
-
Belching
-
Difficulty swallowing
-
Fatigue
-
Heartburn
Additional diagnostics may include:
-
Barium X-ray or CT of the upper digestive tract to identify the location and positioning of the gastric organs
-
Endoscopy exam, during which your doctor passes a thin, flexible tube equipped with a light and video camera (endoscope) down the throat and into the esophagus and stomach to check for inflammation
Hiatal Hernia Treatments
The symptoms associated with hiatal hernia, such as acid reflux, can be treated with lifestyle changes and medication. Surgery may be necessary to repair the hiatal hernia.
Specific treatment for a hiatal hernia will be determined by your doctor based on multiple factors, including your general health, anatomy, extent and location of the hernia, and severity of symptoms such as acid reflux. Any instance in which the stomach or abdominal organs rotate or twist, causing severe pain, blockage and possible strangulation in which blood supply is lost, is always treated with emergency surgery.
Hiatal Hernia Lifestyle and Medication Treatments
Many people do not experience any symptoms related to their hiatal hernia, or their symptoms, like heartburn, are mild. Generally, the symptoms of hiatal hernias can be controlled with lifestyle changes and medication such as:
-
Eating meals at least three to four hours before lying down
-
Eating moderate to small portions of foods
-
Limiting fatty foods, acidic foods (citrus fruits or juices), foods containing caffeine and alcoholic beverages
-
Losing weight or maintaining a healthy weight
-
Over-the-counter antacids or antihistamines; your physician may prescribe a stronger medication to manage your symptoms
-
Sleeping in a slightly elevated position
-
Smoking cessation
Hiatal Hernia Surgical Treatments
Surgery to repair a hiatal hernia is usually performed through small incisions during which the stomach and any other surrounding tissue are pulled down from the chest cavity and back into the abdomen. The surgeon will also make the opening in your diaphragm smaller and may reconstruct an esophageal valve to treat reflux.
Alternatively, hiatal hernia can be repaired through the chest.





