Discoid Meniscus
A discoid meniscus is an abnormally shaped meniscus in the knee that is more prone to injury than typical meniscus. Symptoms often start in childhood.
What You Need to Know
- While discoid meniscus is common, some people do not know they have it and never require treatment.
- Symptoms of discoid meniscus can include knee pain, stiffness or inflammation, limited range of motion, instability, and a locking sensation in the knee.
- For those without symptoms, periodic checkups with a doctor can often be enough to manage a discoid meniscus.
- To address the symptoms, surgery may be needed to reshape a discoid meniscus into a normal crescent, and in rare cases to replace it.
What is a discoid meniscus?
Discoid meniscus is a congenital (birth) anomaly in which a meniscus is abnormally shaped. While a typical meniscus resembles a crescent moon, a discoid meniscus is thicker and looks more like a half or full moon. Its abnormal shape and composition make a discoid meniscus more prone to injury and painful symptoms that may require surgery.
It is estimated that 3% to 5% of the U.S. population have discoid meniscus. However, in many cases it doesn’t cause symptoms, so the actual number of cases is unknown. Studies show that discoid meniscus is more common in Asian countries, compared with other countries.
Discoid Meniscus Injuries | FAQ with Dr. R. Jay Lee
Discoid Meniscus: Information from Johns Hopkins All Children’s Hospital
What causes a discoid meniscus?
While the cause of discoid meniscus is unknown, theories suggest it results from a developmental anomaly that happens in the womb, when the meniscus in the knee deviates from the typical structure.
Types of Discoid Meniscus
Each knee has two menisci, and discoid meniscus can occur in either:
- Medial meniscus (inside of the knee). Discoid medial meniscus is rare.
- Lateral meniscus (outside of the knee). Discoid lateral meniscus is more common than discoid medial meniscus.
In some cases, discoid meniscus affects both knees — this is called bilateral discoid meniscus.
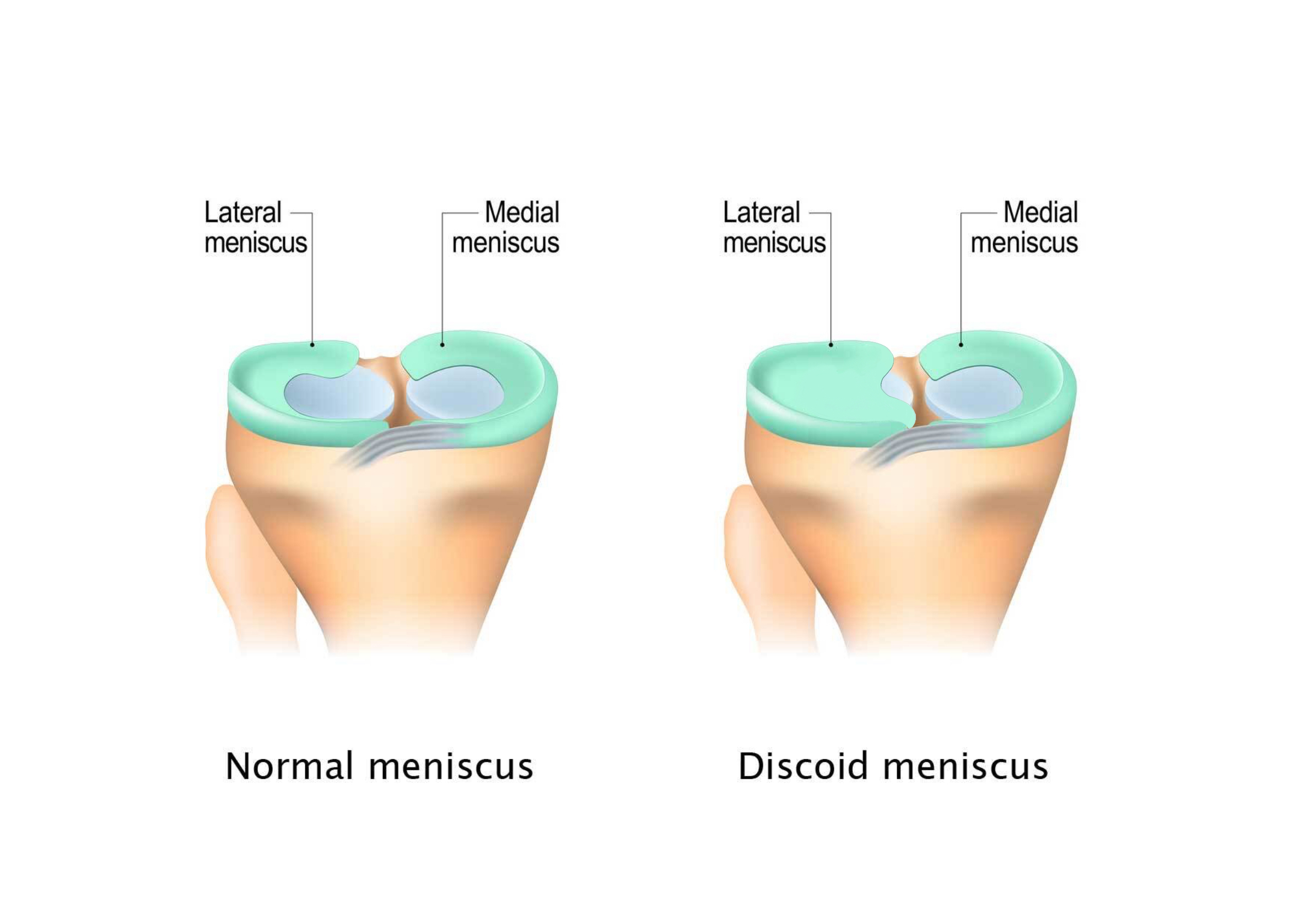 Normal meniscus (left) versus discoid meniscus (right).
Normal meniscus (left) versus discoid meniscus (right).
Discoid Meniscus vs. Normal Meniscus
A typical meniscus is shaped like the letter C — think of a crescent moon. There are several ways a discoid meniscus may differ from a normal meniscus, including shape, stability and the way it is prone to tears.
- Shape – the contour, height and width of the meniscus. Compared with a typical meniscus, a discoid meniscus can be thicker and wider. Based on the shape, there are several types of discoid meniscus:
- Incomplete discoid meniscus – wider than normal, resembling a half-moon
- Near-complete discoid meniscus – mostly rounded with a slight indentation on one side
- Complete discoid meniscus – rounded like a full moon
- Stability – how the meniscus is attached to surrounding structures. In some cases, one or several ligaments that connect the meniscus to the tibia are missing.
- Anterior instability: The meniscus is detached from the front.
- Posterior instability: The meniscus is detached from the back.
- Anterior and posterior instability: The meniscus is detached from the front and back.
- Tears – On a microscopic level, the discoid meniscus fibers are less organized than those of a normal meniscus. Thus, they are more prone to tear at a young age and more prone to retear in the future, including:
- Horizontal tears – tears from side to side of the meniscus
- Vertical tears – tears that go from top to bottom of the meniscus
All these factors are critical to determining the right treatment plan.
What are the symptoms of discoid meniscus?
Many people who have discoid meniscus never experience symptoms. Others may start feeling pain and discomfort within the first two decades of life, due to the discoid tissue gradually wearing down or tearing from use, but the condition can be diagnosed at any age.
Symptoms can include:
- Knee pain and tenderness, usually on the outside of the knee for a lateral discoid meniscus. Sharp pain can be felt when performing high-intensity activities, such as sports that involve running, jumping and pivoting or twisting.
- Popping sensation within the knee
- Stiffness or inflammation in the knee
- Limited range of motion/inability to fully straighten the knee
- Feeling that the knee is unstable or giving out
- Catching or locking sensation when fully bending or straightening the knee
- Weakness in surrounding muscles (thighs and calves)
These symptoms can develop at any time, and do not have to be caused by a traumatic event.
Am I likely to get injured because of discoid meniscus?
A discoid meniscus is more prone to injury than a regular-shaped meniscus due to its larger, irregular shape and weaker tissue. If the discoid meniscus is missing a ligament attachment to the tibia, the risk for injury can be from the lack of stability.
Discoid meniscus injuries can include:
- Meniscal tears
- Meniscal cysts, which occur when a pocket of fluid accumulates around the meniscus in response to injury and tearing
- Parts of the discoid meniscus getting caught in the knee joint, causing it to lock up
Once injured, a discoid meniscus is unlikely to heal on its own because of the weaker blood supply to the tissue, weaker tissue, abnormal structures and instability of the meniscus.
Athletes with discoid meniscus are more prone to injury because their knees often undergo the stress of intense twisting motions, such as in sports that require pivoting or fast changes in direction like soccer, basketball, dancing and football.
How is discoid meniscus diagnosed?
A discoid meniscus that does not cause pain or other symptoms is often discovered during imaging of the knee for other medical issues.
If you are experiencing symptoms, or an injury occurs, schedule an appointment with your doctor.
During the exam, the doctor will test the knee by twisting it in various directions to determine range of motion, if any pain occurs and if popping or clicking sounds can be heard. Often, imagining is needed to confirm the diagnosis.
Imaging Tests
While X-rays can help rule out other problems in the knee and a clinical exam can suggest the presence of a discoid meniscus or a meniscus tear, an MRI scan is the best imaging test for diagnosing discoid meniscus. It can reveal the specific shape of the discoid meniscus, as well as identify tear patterns within the meniscus.
Discoid Meniscus Treatment
People who do not have pain or other debilitating symptoms can go their entire lives without treating a discoid meniscus. Over the years, the knee can adapt to the anatomy and function normally. Periodic follow-ups with a doctor can help detect any signs of deterioration.
If the discoid meniscus is torn and there is no popping, locking and catching, pain can be initially managed with nonsurgical treatments, including:
- Taking over-the-counter medications to reduce pain and inflammation
- Following the RICE regimen — rest, ice, compression and elevation
- Using a cane or another device to keep weight off the knee
- Modifying activity, such as stopping sports or activities that involve jumping or twisting movements
- Participating in physical therapy to help restore mobility, strength and function to the knee and surrounding muscles
Small tears sometimes heal on their own, especially in younger children with a healthy blood supply to the knee, and if the tear is near the rim where the blood supply enters the meniscus. For larger tears, surgery is usually needed to address symptoms and restore knee function.
Discoid Meniscus Surgery
The surgical approach depends on the type of discoid meniscus, the person’s age, severity of symptoms, tear pattern, as well as the width and thickness of the discoid meniscus.
The goal of the surgery is typically to reshape the discoid meniscus while preserving as much of the healthy tissue as possible. This procedure is called saucerization, and it often helps maintain the function and prevent future tearing of the meniscus.
If the discoid meniscus is torn, abnormal damaged parts are removed and the meniscus is reshaped. If the periphery of the meniscus is torn or unstable, it may need to be repaired to try to preserve normal meniscal function. Removal of the meniscus may be necessary in severe cases when it is damaged beyond repair. Discoid meniscus removal poses greater consequences for children, such as a higher risk of osteoarthritis in the future. The meniscus serves as a shock absorber, protecting knee cartilage. Without a meniscus, cartilage can get damaged and wear out sooner. Therefore, in most cases that involve children, repair should be attempted before considering the removal of discoid meniscus.
Discoid meniscus surgery is often done arthroscopically, meaning a few small incisions are made to insert a small camera and surgical instruments.
Recovery After Discoid Meniscus Surgery
After the surgery, your doctor will provide instructions for recovery, which may include:
- Pain medication to reduce swelling and manage pain (could be prescribed or over the counter).
- Bracing to increase stability and reduce pressure on the menisci.
- Assistive devices, such as crutches or a wheelchair, to avoid putting weight on the recovering knee.
- Physical therapy to help restore muscle strength and range of motion in the knee.
- Activity modification, such as avoiding jumping, twisting and high-impact activities that can disrupt healing.
Normal activities and sports can typically resume within a few weeks or months after the surgery.