Brachial Plexus Surgery
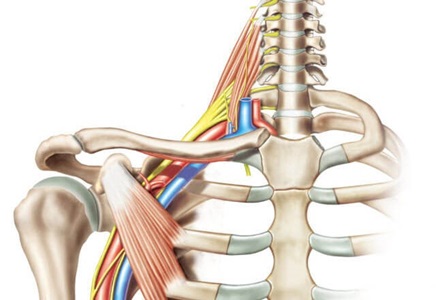
The brachial plexus is a network of nerves that conveys movement and sensory signals from the upper spinal cord in the neck down into the arms and hands. Trauma to the neck or shoulder can injure the brachial plexus, causing pain, numbness, weakness or paralysis in the arms or hands.
Some brachial plexus injuries heal on their own and leave the person with normal or near-normal function. For more severe injuries, brachial plexus surgery may be the best chance to relieve pain and restore sensation and mobility.
Who may need brachial plexus surgery?
- People with a neck or shoulder trauma that resulted in severed, torn or severely stretched nerves in the brachial plexus.
- Those with continuing, debilitating pain or loss of function in the arm after a trauma or because of nerve damage during surgery.
- Those with scarred nerves that form tumors called neuromas.
- People with nerve tumors of the brachial plexus that were not caused by trauma, such as schwannomas and neurofibromas.
Getting Ready for Brachial Plexus Surgery
Before recommending surgery, the surgeon needs to understand which nerves are affected and the injury’s location and severity. If you need brachial plexus surgery, a multidisciplinary team of neurosurgeons, plastic surgeons and neurologists will work with you to determine the best treatment approach based on the injury and your treatment goals.
The surgeon takes an in-depth history, noting your general health and details on when and how the injury happened. The surgeon will ask you about your symptoms and how they impact your work, daily activities and quality of life.
Details about weakness or paralysis, loss of sensation, and the quality of pain (dull, stabbing, burning, stinging, etc.) can provide important diagnostic clues on the location and severity of injury to the brachial plexus nerves.
During a physical examination, the surgeon will compare motor function, sensation and pain in the affected limb to your unaffected side. The surgeon may use video to record part of the exam so he or she can refer to it during surgical planning.
Imaging studies help the surgeon determine the extent and location of the injury and to plan surgery accordingly. Ultrasound and MRI show damaged nerves and soft tissue. Computerized tomography (CT) and X-rays reveal broken bones in the neck, shoulder or arm. Arteriography identifies damaged blood vessels.
Electromyography (EMG) is essential for testing nerve function. An EMG provides important information about the location and degree of nerve damage, whether the nerves and muscle are recovering, and which unaffected nerves can potentially be used to restore function if surgery is needed.
The surgeon works with you to focus on the most distressing or debilitating symptoms or issues caused by the injury. In planning your surgery, these considerations help customize the approach and address your specific needs.
When is the best time for brachial plexus surgery?
Those who have a traumatic brachial plexus injury due to a penetrating object, such as a knife, may need surgery right away to re-connect the nerves.
In other cases, when brachial plexus nerves have been crushed or stretched, the surgeon may monitor you for several weeks or months to see if the injury heals or improves on its own. EMG studies help determine the progress. You may be referred for physical therapy to ensure that the joints and muscles in your neck, shoulder and arm remain flexible. If the nerves don’t appear to be recovering, surgery may be needed to restore movement and sensation. In this case, having the procedure three to six months after the injury offers the best chance for successful restoration of function.
Waiting too long (two years or more) to have surgery can cause the muscles in the neck, arm and shoulder to permanently shrink (atrophy). In such cases, functional muscle transfers or tendon transfers may be necessary to restore function.
Types of Brachial Plexus Surgery
The goal of brachial plexus surgery is to relieve your pain and restore sensation and motor function to your shoulder, arm and hand. Surgical approaches consider the type, location and extent of nerve injury, as well as your overall health and the impact of injury on your ability to work and quality of life.
Procedures your surgeon might recommend include:
Brachial Plexus Nerve Repair
When a nerve has been cut or torn, the surgeon may be able to re-connect it by sewing the ends back together. This is performed with the help of a microscope and small, specialized instruments.
Brachial Plexus Decompression and Neurolysis
When a nerve is compressed but otherwise intact, a decompression surgery can help relieve the pressure on the nerve and address related symptoms and loss of function. This can be done by removing scar tissue or adhesions (a procedure called neurolysis) from around the injured nerve.
Nerve Grafting Surgery for Brachial Plexus Injuries
When a nerve has been injured or scarred severely, it may no longer be able to carry signals from the brain to the arm and hand, leading to paralysis. In this case, surgeons can remove the damaged nerve segment and replace it with a segment of an expendable sensory nerve from another part of the body, such as the sural nerve in the leg. This procedure, called a nerve graft, helps create a bridge that replaces the injured portion of the nerve and provides a pathway for nerve regeneration.
Brachial Plexus Nerve Transfer Surgery
During a nerve transfer, a nearby functioning nerve that is performing a noncritical function is connected to the injured nerve. This creates a framework for new growth and a pathway for signals. In many cases, a nerve transfer procedure provides the best chance of restoring movement and sensation to the muscles and skin.
Nerves that can be transferred this way to treat brachial plexus injuries include the medial pectoral nerve in the front of the shoulder, the intercostal nerve under the ribs, the musculocutaneous nerve in the arm, and many other nerves in the forearm and hand. The optimal nerve to use for a transfer depends on which nerve is injured and the location of the injury. As with all types of brachial plexus surgery, time is of the essence for nerve transfers because there is a limited window for restoring nerve supply to the affected muscles before irreversible atrophy occurs.
Tendon Transfer Surgery for Brachial Plexus Injuries
During a tendon transfer, a functioning and expendable tendon is attached to a tendon that is paralyzed as a result of brachial plexus injury. After tendon transfer, the functioning tendon will pull on the once paralyzed tendon to restore lost movement in an upper extremity.
In some cases, a tendon transfer offers the best option for restoring movement after a brachial plexus injury. The most common reason for the procedure is that too much time has passed after the injury and nerve grafting or transfers are no longer options. Unlike nerve transfers, tendon transfers can take place any time after the brachial plexus injury.
Functional Muscle Transplant for Brachial Plexus Injuries
Functional muscle transplant is another option to restore movement when too much time has passed after the brachial plexus injury and when nerve repair, grafting or transfer is no longer possible. A nonessential muscle, such as the gracilis muscle of the inner thigh, is transplanted to replace a nonfunctioning muscle in the shoulder, upper arm or hand. Blood flow is restored to the transplanted muscle by connecting tiny blood vessels under a microscope. A nearby nerve in the upper extremity is used to provide motor function for the transplanted muscle. Like tendon transfers, functional muscle transplantation can take place any time after the brachial plexus injury.
Brachial Plexus Injury Treatment at Johns Hopkins
Our experts at the Johns Hopkins Peripheral Nerve Surgery Center are well-versed in all types of brachial plexus injuries, from birth injuries to radiation treatment complications. We use a holistic approach, creating an individualized treatment plan for each patient.
During Brachial Plexus Surgery
- Most surgical procedures to repair brachial plexus nerves are performed with the patient under general anesthesia.
- As the surgeon works, the team monitors your nerve function using a technology called evoked potentials.
- The specific procedures performed during brachial plexus surgery often depend on what the surgeon discovers when he or she examines the injury up close. These findings provide detail on the extent and severity of the nerve injury.
Recovery After Brachial Plexus Surgery
Recovery after brachial plexus surgery includes healing of the tissues that were operated on and recovery of lost function. While healing of the tissues is relatively quick, function recovery may take months depending on the procedure you had and the extent of the injury.
After surgery, you may need to use a sling or splint to keep the affected arm in the appropriate position for healing:
- For some nerve transfers below the elbow, a splint may be needed for two weeks.
- Nerve repairs, transfers and grafts above the elbow typically require a sling for only two weeks.
- For tendon transfers and functional muscle transplantation, a sling and/or splint is likely required for one to three months. During this time, you may start physical therapy.
Physical therapy is critical to help you recover after brachial plexus surgery. The type of therapy, timing and duration depends on the type of surgery.
Brachial Plexus Surgery Success Rate
After nerve repair, grafting and transfer, a period of nerve regeneration is required before movement and sensation improve. This can take months to years, depending on the type of surgery performed. Tendon transfers take weeks to heal and then require rehabilitation to regain function. Typically, tendon transfers heal quicker but offer less functional results.
The success of your procedure depends on the severity of the injury and the expertise of the surgeon and team. For patients having nerve transfers, 80% to 90% see improvement in function. For other procedures, depending on the patient’s age and the nature of the injury, the percentage may be lower. Choosing a surgical team with specialized experience and skill in brachial plexus surgery can improve the chance of a good outcome.






